The importance of nurses educating patients is well known and documented in studies showing that patient education results in greater patient compliance and leads to better health outcomes. Moreover, healthcare is increasingly shifting towards patient- and consumer-centered healthcare. Self-care by patients requires education as part of standard nursing practice, using strategies such as family education.
What is patient education?
Patient education takes place through patient teaching, when nurses teach, influence, and empower patients to manage and perform aspects of medical care on their own confidently. Patient education is one of the most important parts of nursing care. It encourages patients to focus on their health status and better communicate their feelings and desired health outcomes to their family members. Teaching patients and their families also allows nurses to feel satisfaction in nursing care, with positive outcomes for nurses, such as nurse job retention.
Some areas of patient education are:
- certain care procedures, such as changing a bandage
- disease management, such as insulin injections
- explaining discharge instructions
- pre-operative and post-operative instructions
- sharing of printed patient education material or digital resources
What is the nurses’ role in patient education?
Nurses teach patients the essential skills they need for self-care. With patient teaching, the nurse is a guide and support and is responsible for how the patient continues nursing care after leaving the care setting. The benefits of better patient education include improved health outcomes, patient safety, and reduced levels of readmission.
There is an important surge among nurses who wish healthcare executives and insurance providers would recognize patient education by nurses as an independent, reimbursable skill. When the nurse’s role in patient education is recognized, clinical nurses will:
- Pay greater attention to ensuring patient education takes place and
- focus on patient teaching for different patient groups effectively (such as different ages and differing learning abilities), resulting in better patient outcomes.
The importance of nurses educating patients: 10 Tips for Success
Nurses are the link between healthcare providers in the care setting and patient engagement as patients participate in their care following discharge. Nurse leaders who are teaching patients can improve patient education by ensuring they adhere to these patient education tips:
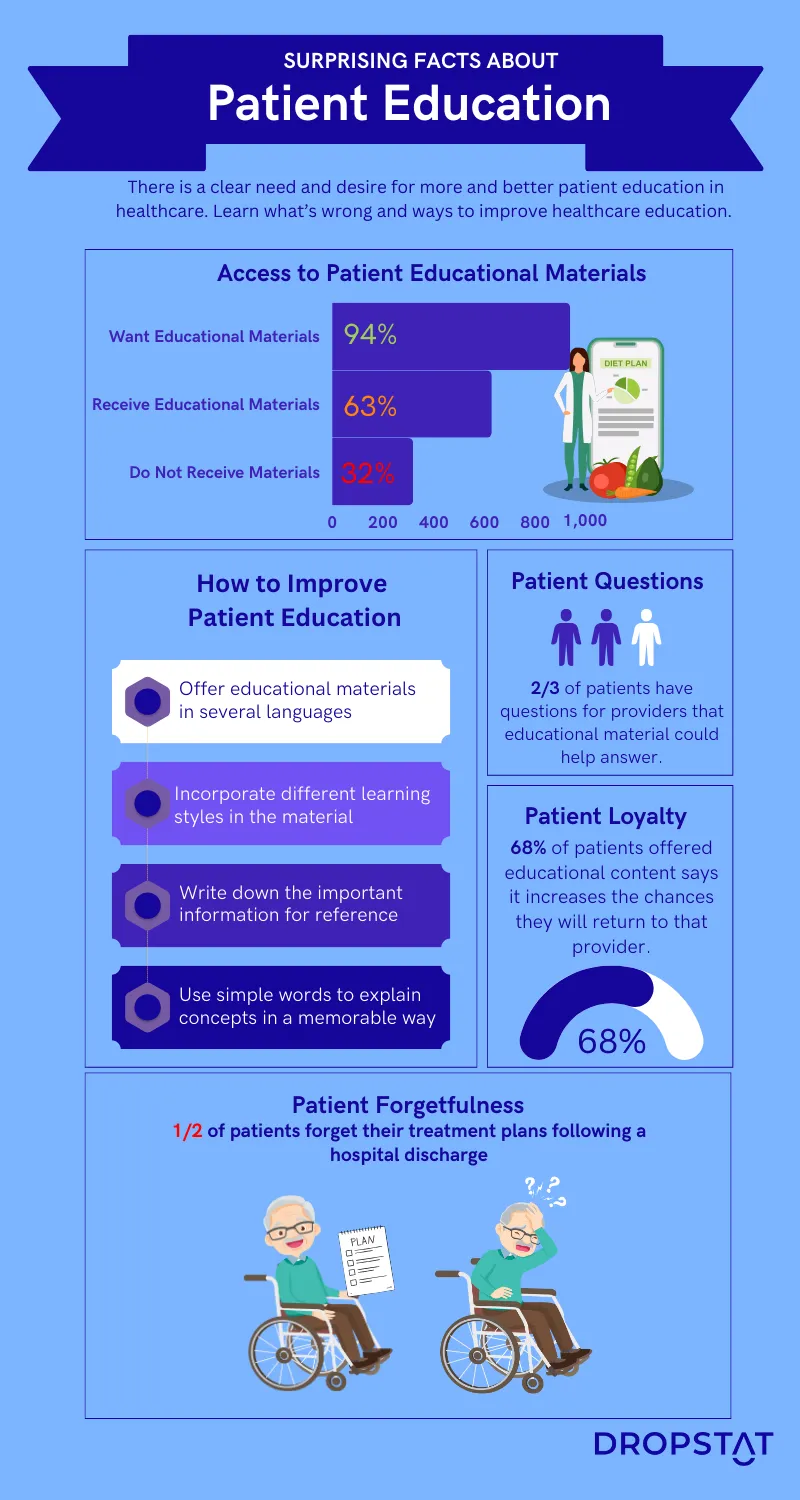
1. Provide patient education materials in the patient’s native language
Patient education is more effective when teaching patients the material without language barriers in healthcare.
2. Use the patient’s preferred learning style for patient education
The 4 predominant learning styles when teaching patients are visual, auditory, read/write, and kinaesthetic. This means patient education for some patients will include lists of instructions, others will do better watching videos online, and some will prefer to experience a demonstration and try it themselves. In practice, patient education should include a combination of several modalities.
3. Leverage technology to improve health literacy
Provide a list of patient education websites and technologies that patients can access that can contribute to their optimal care and patient outcomes.
4. Stimulate the patient’s interest before and during patient education
Nurses should explain how effective patient education will help towards recovery. Nurses should smile during the patient education process, address patients by their preferred name, make eye contact, and say what they are going to explain/demonstrate before they do it and after they do it.
5. Consider the patient’s limitations when offering patient education
Patient education for patients with limitations may require providing documentation in large print, asking the patient if they understood what the nurse said to them, and asking them to tell it back to the nurse or answer questions about self-care.
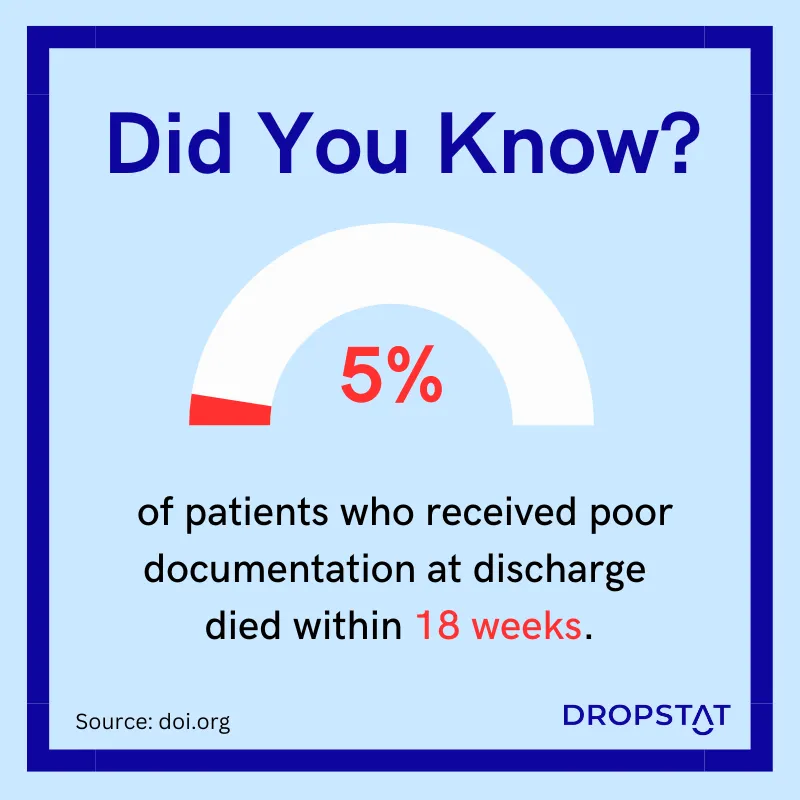
6. Health educators should write down the important information
A study on patient education found that 5% of patients perished within 18 weeks of receiving low-quality documentation at discharge. At the end of a patient interaction, many patients are tired or emotionally drained, and it is easy for them to forget important information.
7. Include family members in health education events
Including family members as part of the patient education process means providing “family education.” Practically, family education includes addressing the patient and their adult children. Family education is a shared learning process that can significantly improve patient recovery.
8. Use telehealth in patient-education nursing to reach patients
Telehealth nursing means you can maximize patient exposure to effective care to offer patient education between visits or to avoid exposure to health risks of in-person visits.
9. Improve accessibility in health education
Provide descriptions of the text through images and verbal discussion. Sometimes, humor can be used in patient education to break through communication barriers.
10. Redesign health literacy documentation for simplicity
Plainlanguage.gov recommends simplicity and clear English to get your message across more quickly to more patients in less time for more effective patient education.
The importance of nurse supervision of patient education
While patient and family education is critical for reducing the burden on the health system, nurse supervision is important for effective patient education to reflect that progress back to the patient.
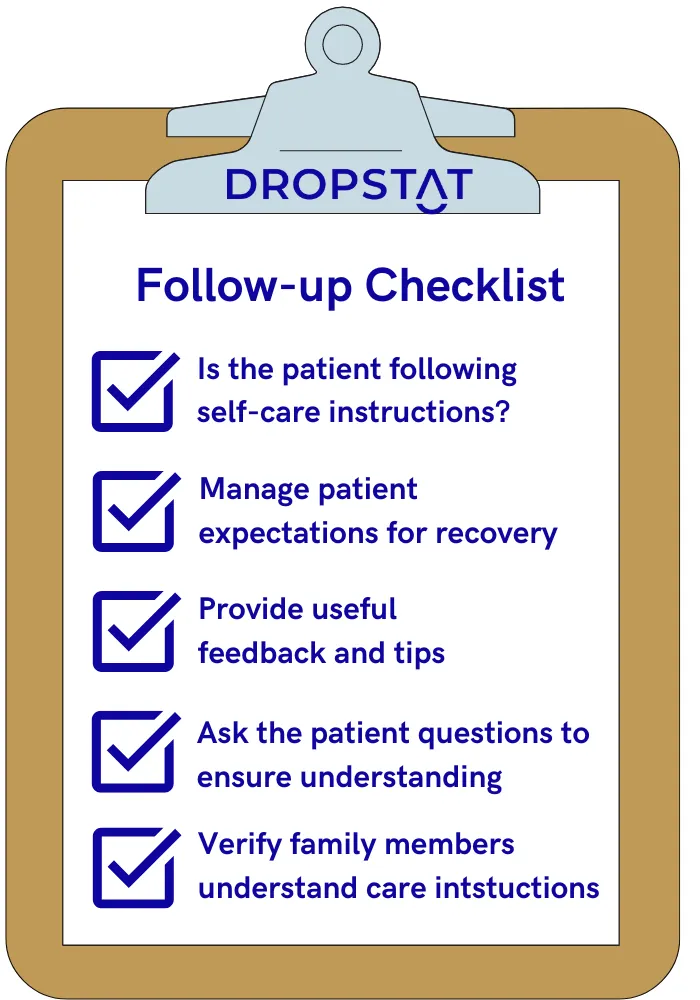
In follow-up patient teaching appointments, nurses should:
- ask how the self-care process is going
- provide helpful feedback and additional tips to patients
- manage patient expectations for recovery
- ask questions to the patient and family to make sure the patient understands the instructions
- check in with family members to ensure the burden of care is not taking a toll on them.
Improving the quality of patient-education nursing
Are there ways to improve the quality of patient education from nurses? Yes. Improvement is always achievable. Nurses’ role as leaders for patient self-care may have changed. Patient teaching is less about disease-oriented patient education and more about “empowering patients to use resources” they have or can access easily.
Here are suggestions for ways to improve patient education by nurses:
- Remove economic barriers. While managers deem that nurse leaders should automatically offer patient education, nurses request financial recognition of the patient education process as a unique skill.
- Health promotion skills. Provide patient teaching courses through seminars and in-service training sessions for nurses to improve their pedagogical abilities.
- Specialist nurse educators. The provision of dedicated nurse educators would allow nurses to share patient education strategies more efficiently and effectively.
- Facilities for patient education. Patients and educators can benefit from a dedicated educational environment with the provision of reading material and access to patient teaching and online education resources.
Dropstat recognizes the importance of nurses educating patients and offers a practical solution
Dropstat is an AI-powered nurse scheduling app that supports nurse schedulers as they engineer sufficient and safe staffing in every unit in a healthcare facility – in every shift. Part of the job of the scheduler is to ensure that nurses of the correct discipline are present for every shift as patient acuity demands. Patient well-being and outcomes are greatly improved by combining nursing and patient education by employing nurses who are qualified to teach patients. The benefits of this include improved patient outcomes and reduced levels of readmission.
Using Dropstat ensures you can place nurses who recognize the importance of nurses educating patients on every shift that it is relevant.
Schedule a demo to see how the nurse’s role in patient education can benefit your facility and your patients.







