Additionally, healthcare compliance standards strive to ensure that healthcare facilities prevent fraud, waste, and abuse by implementing the right processes, hiring qualified personnel, and utilizing the resources required to effectively uphold institutional standards. However, this task is not simple and requires continuous attention to the evolving protocols.
With this challenge in mind, Dropstat has created an AI-based platform that emphasizes compliance through safety standards, increased communication among healthcare teams, and facility-specific staffing techniques based on HPPD calculations and union compliance. These features position your facility to meet protocol and regulatory standards even with the most challenging labor obstacles.
Dropstat’s methods to simplify compliance in healthcare
Dropstat knows that healthcare compliance is a prerequisite for efficient operations and is critical while implementing state-of-the-art technology for healthcare. One main compliance challenge that Dropstat targets is safe staffing ratios within clinical settings. The platform helps facilities calculate hours per patient day (HPPD) to determine the disciplines and number of nurses necessary to adequately care for the patient volume at that time.
Additionally, Dropstat’s AI and incorporated chat feature improves care-team communication, simplifying staffing practices by enabling schedulers and administrators to communicate more widely with internal and agency staff members. This allows healthcare facilities to take on a proactive approach to shift scheduling that works in the best interest of the staff and patients. Dropstat offers care teams many avenues to promote safe, healthy working conditions that align with the main standards of compliance that regulate the healthcare industry, such as HIPAA and OSHA.

Different components of healthcare compliance regulations
The complexity of effective healthcare compliance programs is caused by the various different requirements designated by local, state, and national standards. Some cities, such as Los Angeles, offer supplementary insurance coverage (like the L.A. Care Health Plan) in an effort to bolster rates of insured individuals and families. With these programs in place, it is crucial that surrounding healthcare facilities are aware of the programs’ provisions and how they may impact the practices and demographics of patients.
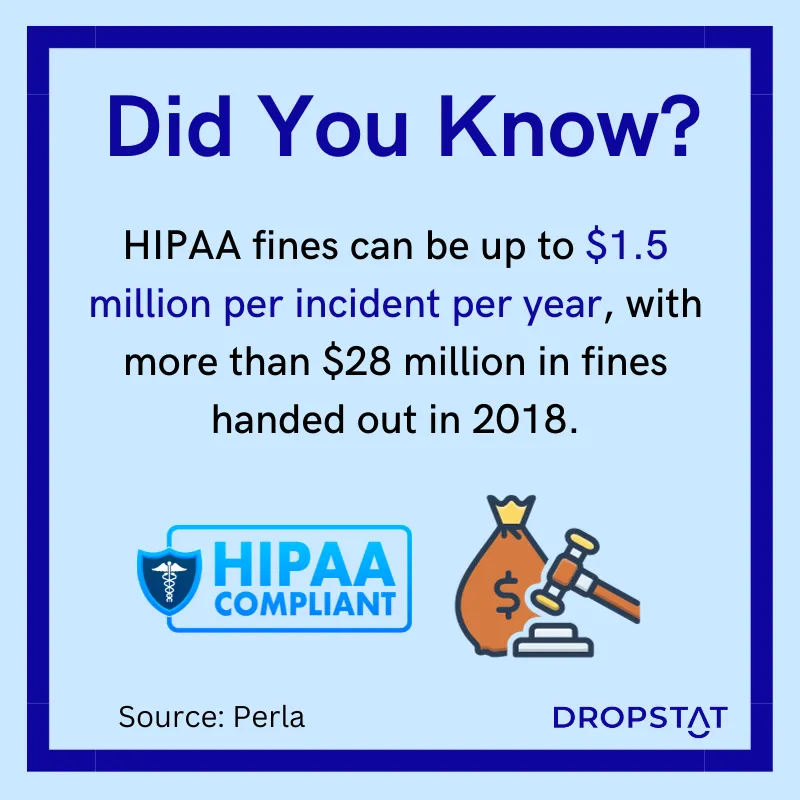
One serious risk that healthcare institutions must be aware of is the renewal period for medical licenses, which vary by state. Failing to ensure that all clinicians in your facility have valid licenses can result in significant legal penalties, fines, and a poor public image. Perhaps most importantly, federal regulations determine guidelines for patient health information safety as well as shift compensation and finances. One federal law in particular, HIPAA, mandates that sensitive patient health information is secured and will not be divulged without permission from the patient.
Promoting risk management for effective healthcare compliance
Establishing an effective compliance program for your facility will definitely support risk management efforts while improving Medicare ratings and public reporting metrics. A few of the top measures that Medicare uses to report on compliance are:
- Staffing levels based on inpatient census
- Staff turnover
- Infection control citations
However, the government is not the only entity that strives to promote compliance. Most healthcare organizations determine their own internal compliance standards that outline procedures to reduce nurse bullying, improve communication and patient-provider interactions, and adhere to high-quality care.
Some common forms of compliance that govern the healthcare industry include:
Union Compliance
One major obstacle within healthcare is ensuring union compliance, specifically with regard to shift duration and working conditions. The inevitability of shifts that are short-staffed often leads to nurses working overtime which likely reduces the quality of care given to patients.
HIPAA
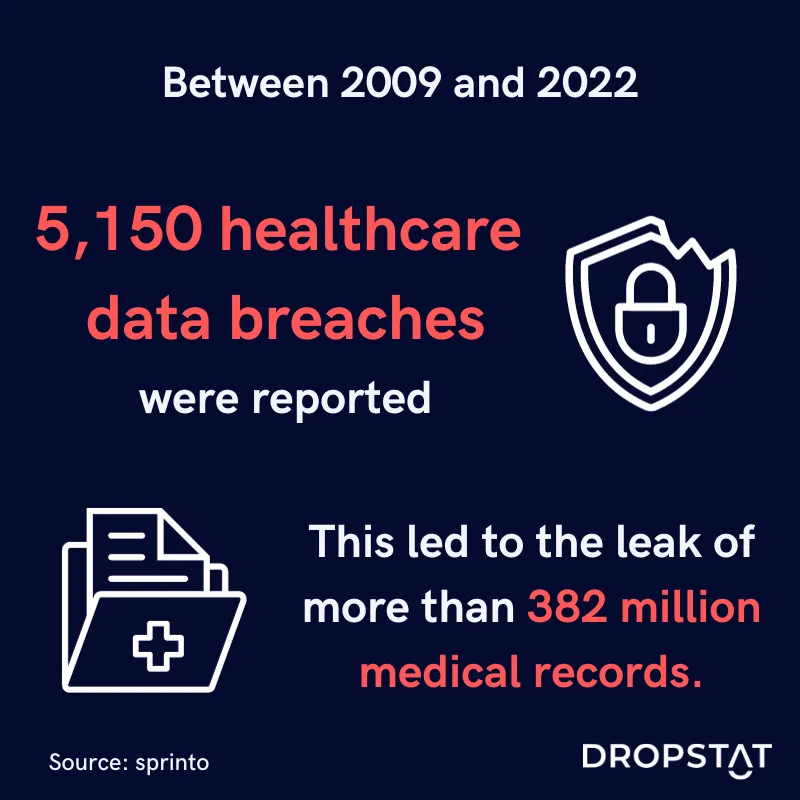
The healthcare industry generates colossal amounts of data, which requires a method to keep that data secure and organized. The main objectives of the Health Insurance Portability and Accountability Act (HIPAA), are to ensure security standards for patient privacy (especially with the increased use of electronic health records), to assist in decreasing costs as a result of administrative tasks, and to secure continued healthcare coverage.
This federal law prioritizes keeping patient health information safe that could be used to identify patients without their knowledge. Compliance with HIPAA is mainly focused on security and privacy associated with health information.
OSHA
Working conditions within healthcare settings are a serious concern for many healthcare professionals who are in hazardous situations regularly. The Occupational Safety and Health Administration (OSHA) institutes measures to reduce the risk of harm within the workplace by providing educational resources and implementing training programs and protocols such as handling blood-borne pathogens, COVID-19 infection control, enforcing proper workplace dress codes, and personal protective equipment. Compliance with these regulations promotes safer working environments that keep your staff feeling protected and valued.
HITECH
The HITECH Act promotes the objectives of HIPAA through its emphasis on protecting the exchange of electronic health data while enhancing healthcare interoperability between different entities. Given the ability to share patient health information among healthcare providers, the HITECH ACT creates procedures to enforce safer data-sharing methods and improve care coordination among the healthcare team.
EMTALA
In 2020, nearly 40 of every 100 U.S. people sought emergency care. Given that emergency departments are often the first line of defense for many individuals who are unable to access primary care, the Emergency Medical Treatment and Labor Act (EMTALA) outlaws turning patients away from emergency departments if they are seeking emergency care. If a healthcare institution is in violation of EMTALA, the organization may incur fines and will no longer be eligible to receive Medicare funding.
Who is responsible for your facility’s healthcare compliance?
One of the main bodies of compliance within the federal government is the Office of the Inspector General within the Department of Health and Human Services (DHHS). This agency works alongside institutions served by Medicare and Medicaid to avoid fraud, abuse, and waste while strengthening the healthcare programs that serve at-risk populations.
However, on a more organization-specific level, chief compliance officers are tasked with creating internal policies that prioritize compliance through continuous training, accreditation, financing and reimbursement procedures, and processes that allow employees to report compliance risks or concerns. They also produce compliance plans that steer your organization toward safer, more efficient practices while evaluating current procedures to find compliance discrepancies
5 ways to improve healthcare compliance in your facility
Identifying methods to improve your healthcare compliance programs will simplify your facility management processes in many ways. Let’s explore a few ways your facility can improve its healthcare compliance programs.
- Designating a compliance officer
The main role of healthcare compliance officers is to create and execute compliance programs within healthcare facilities and monitor the programs’ success. Compliance officers may also be responsible for educating staff and investigating potential organizational compliance risks.
2. Create clear and effective policies
Establishing policies that are explicit contributes to standardization across your organization. Not only does it create structure, but it also ensures that those policies have the greatest chance of leading to effective organization-wide compliance practices.
3. Conduct compliance audits
Instituting a healthcare compliance program is a great start. However, the compliance plan may not consider the primary risk areas within your organization. For example, many healthcare organizations experience issues related to nurse-to-patient staffing ratios and fraud which can be mitigated by assessing specific departmental operations. Most importantly, however, compliance audits ensure that your facility aligns with state and federal regulations.
4. Implement oversight of staffing practices
One of the greatest healthcare challenges facing us today is the labor shortage. A report from nurse.org found that nearly 42/50 states will likely be at a deficit of nursing staff. With this crisis looming, it is crucial that healthcare organizations ensure that they have enough staff with the right skills to deliver safe care to each of their patients. Practicing early staffing, prioritizing senior nurses, and reducing reliance on agency and overtime staffing are all methods that can improve your care delivery with the right oversight.
5. Offer continuous compliance training for your staff
Compliance education guarantees that your workforce understands the state and federal standards that govern healthcare, including patient privacy, staffing standards, and workplace safety. Prioritizing staff education within your organization is an ongoing process that reduces potential risks, strengthens overall compliance, and protects patients.
Conclusion
It is evident that compliance guidelines increase patient safety and health outcomes and strive to protect nurses and healthcare workers from burnout and hazardous work environments. Ultimately, prioritizing these aspects of healthcare will improve your facility’s CMS Care Compare quality ratings, improving your public image and increasing revenue.
Founder and CEO of Dropstat, Sara Well, explained that “Healthcare organizations are held accountable to adhere to union standards of workforce management without the tools they need to do so. By aligning our technology with fair labor standards, our clients don’t have to put any thought towards ensuring that internal staff with seniority status (for example) are prioritized. They can focus more attention on ensuring that safe staffing ratios are a key focus and let the technology manage compliance algorithms. This enables safer patient care and happier staff with lower burnout rates.”
Schedule a demo now to join Dropstat in their effort to create a new era of safe staffing.







