Alarm fatigue develops in nurses because of the multitude of incessant auditory alarms throughout a nurse’s shift. Nurses complain that they ‘hear’ alarms when they go home for the day and even in their sleep. Often, these are false alarms. Is it surprising that the mind shuts out the overflow of auditory information? However, the outcome can be tragic, with the U.S. FDA reporting over 500 deaths related to alarm fatigue in just 5 years. Alarm management is becoming increasingly important.
What is alarm fatigue?
Alarm fatigue in healthcare is when nurses and clinicians become desensitized to medical device alarms and monitor alerts and fail to hear them or respond appropriately.
What causes alarm fatigue?
Alarm fatigue in nurses typically occurs when a health worker is over-exposed to audible alarms. False alarms are a major cause of alarm fatigue.
Alarm fatigue can occur in many fields, but reducing alarm fatigue for patient safety has become a primary goal in healthcare. The Joint Commission chose alarm management as a 2021 National Patient Safety Goal. The APSF (the Anesthesia Patient Safety Foundation) states the goal of reducing alarm fatigue is “to clearly and accurately indicate potential hazards and minimize false or nuisance alarms.”
Alarm fatigue in nursing: better alarm management or hypervigilance?
Instances of alarm fatigue have been tracked for over a decade. False alarms, nonactionable, and nuisance alarms make up 85-99% of audible alarms that do not require clinical intervention, said the Joint Commission already in 2013. Since then, the healthcare community has been working to improve alarm fatigue.
Boston Medical Center (BMC) has focused on improving nurse alarm fatigue since 2012. By applying a multidisciplinary program of alarm management, BMC reduced false alarm signals for patient cardiac monitors from around 1,000,000 signals a week to 400,000.
Xiao and Seagull, who produced a Taxonomy of Alarms identifying three types of false alarms, challenge the “better safe than sorry” approach. It yields too many ‘critical alarms,’ causing alarm fatigue and putting alarm management in the spotlight.
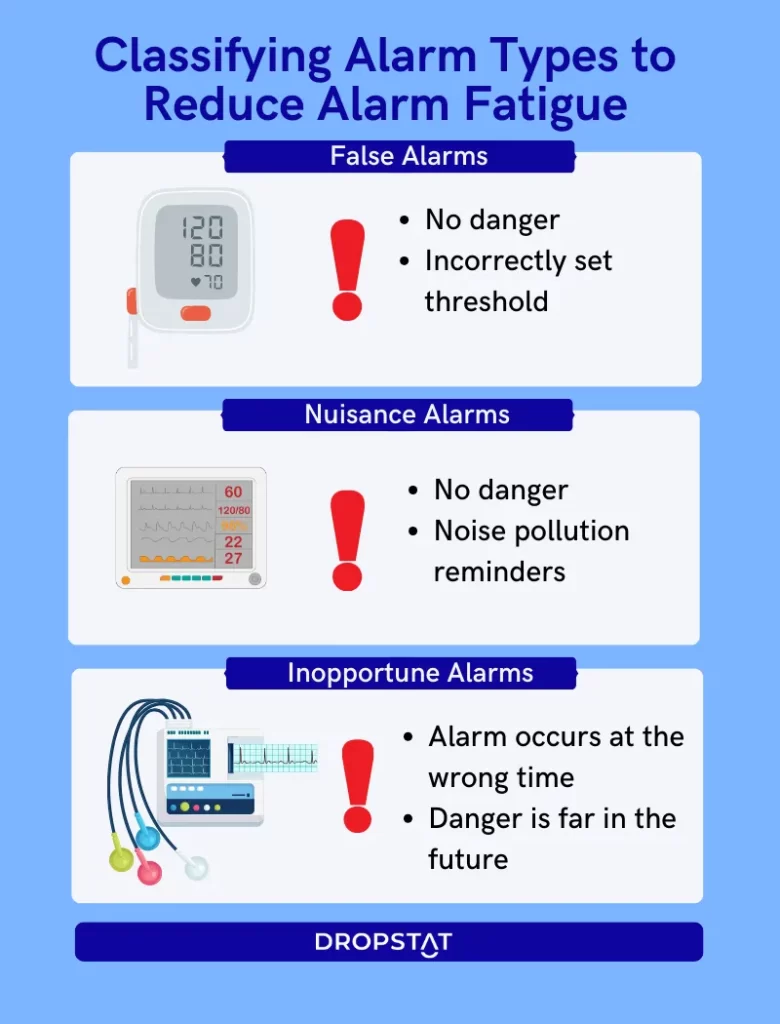
To reduce alarm fatigue, Xiao and Seagull identified types of alarms:
- False alarms – no danger exists; threshold incorrectly set
- Nuisance alarms – no danger exists in the specific medical context
- Inopportune alarms – alarm occurs at the wrong time; the condition is far in the future
Alarm fatigue and the implications for patient safety
Alarms and monitors in healthcare alert workers to potential risks to patient safety. Monitors ‘keep an eye’ on patients 24/7 and relieve critical care nurses of constant supervision. Clinical alarms include all types of alarms incorporated into clinical devices, such as pulse oximeters, cardiac monitors, fetal monitors, apnea monitors, infusion pump alarms, ventilator alarms, and emergency assistance alarms.
Poor alarm management policies and alarm fatigue directly impact patient safety. Alarms are an essential element in the harmony between healthcare consumers and providers:
- Consumers expect optimal levels of vigilance, and critical care nurses are answerable to their superiors, patients and their families, and their consciences. Alarm fatigue causes missed alarms.
- On the other hand, healthcare CEOs must protect critical care nurses’ well-being, improve patient safety, and enhance the financial well-being and reputation of the healthcare facility. Alarm fatigue challenges nurses’ employee wellbeing.
5 Recommendations to Reduce Alarm Fatigue and Improve Nursing and Patient Safety
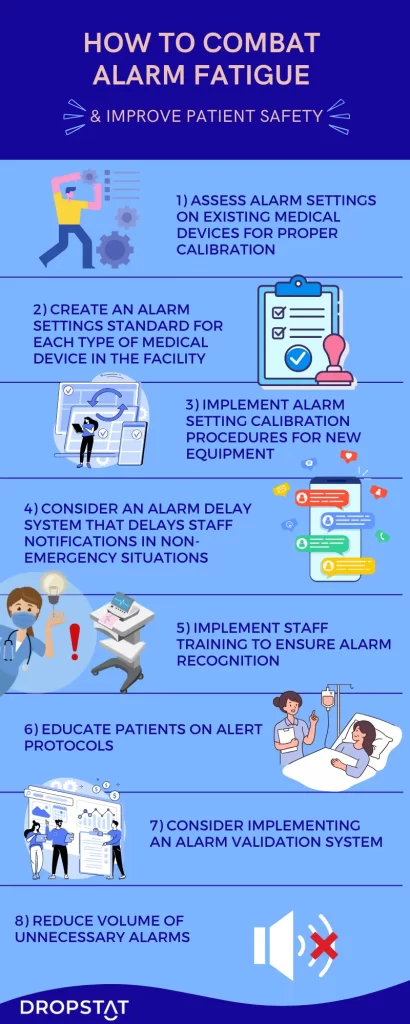
The APSF and other resources offer evidence-based practice recommendations for better alarm management policies in healthcare:
1. Assess Situational factors for alarm fatigue
Conduct an assessment of situational factors, such as lighting, ambient noise, and competing task demands, to understand the challenges of your critical care nurses’ alarm fatigue. Understand your facility’s acoustics and noise pollution factors, including false alarms.
2. Alarm fatigue from new monitors
Assess new equipment for alarm features that decrease a clinician’s workload and do not distract them from other tasks. Investigate how new equipment fits into your culture of safety and other alarm fatigue solutions.
3. Staff training to avoid alarm fatigue
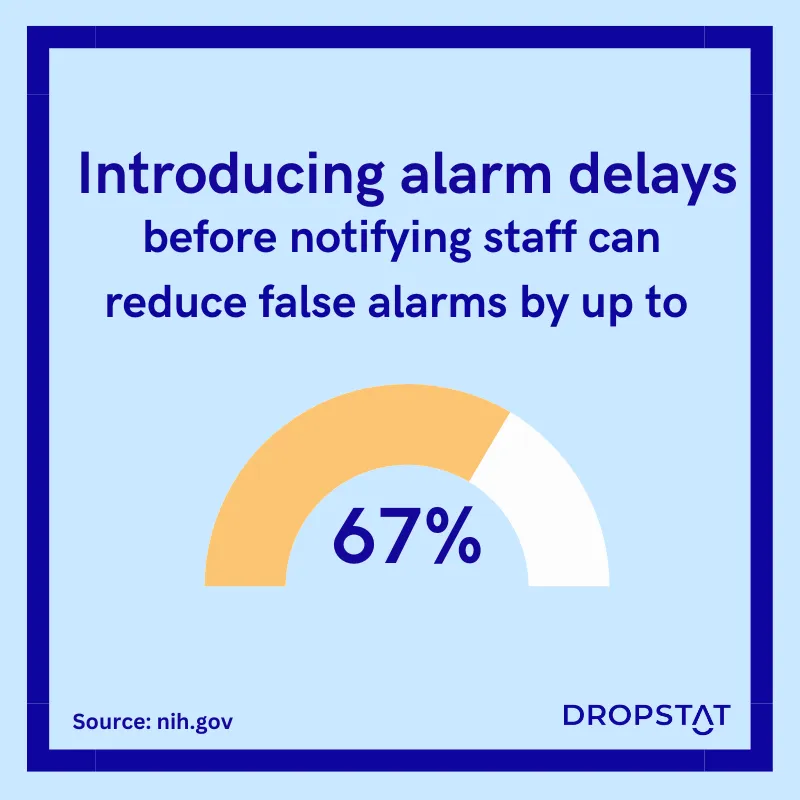
Conduct continuous staff training to enable staff to use equipment at its maximum potential by understanding how to use all alarm settings. For example, nurse leaders should know how to set monitors to delay alarm activation in the case of clinically irrelevant events. All critical care nurses should know how to alter alarm volume and avoid false alarms.
4. Leaders against alarm fatigue
The CEO, the facility manager, nurse leaders, and the director of healthcare quality should follow studies and updates on alarm fatigue and liaise on a regular basis to discuss alarm management and alarm management policies.
5. A patient safety alarm fatigue ‘team’
Where possible, incorporate patient care with nurses educating patients. Educate patients and their families in auditory signal protocols so they know the signals of a real emergency and signs of false alarms. Post notices around hospitals with information about critical alarms and false alarms.
Dropstat conclusion on alarm fatigue in nursing
With practical recommendations for better alarm management, healthcare facilities can reduce alarm fatigue and patient safety. This is possible within an effective safety culture that protects nurses’ well-being, improves patient safety, and enhances the healthcare facility’s reputation. Improvement in finding alarm fatigue solutions will benefit healthcare providers and consumers.
Alarm Fatigue FAQs
Is there a relationship between alarm fatigue and burnout in nurses?
There is a relationship between alarm fatigue and nurse burnout. The NIH reports that 72-99% of alarms are false. False alarms lead to stress for nurses and nurses tuning out alarms. 59% of nurses consider these alarms to be “nuisances” that occur because the equipment was not set to a sensible threshold. Nurses get burned out when they constantly have to respond to unnecessary alarms, and they work with constant fear that a missed alarm might be a close call or an actual emergency. The continuous burden of response wears down nurses’ emotional and sensory reserves, leading to burnout and reduced feelings of personal accomplishment.
What is the greatest risk of alarm fatigue?
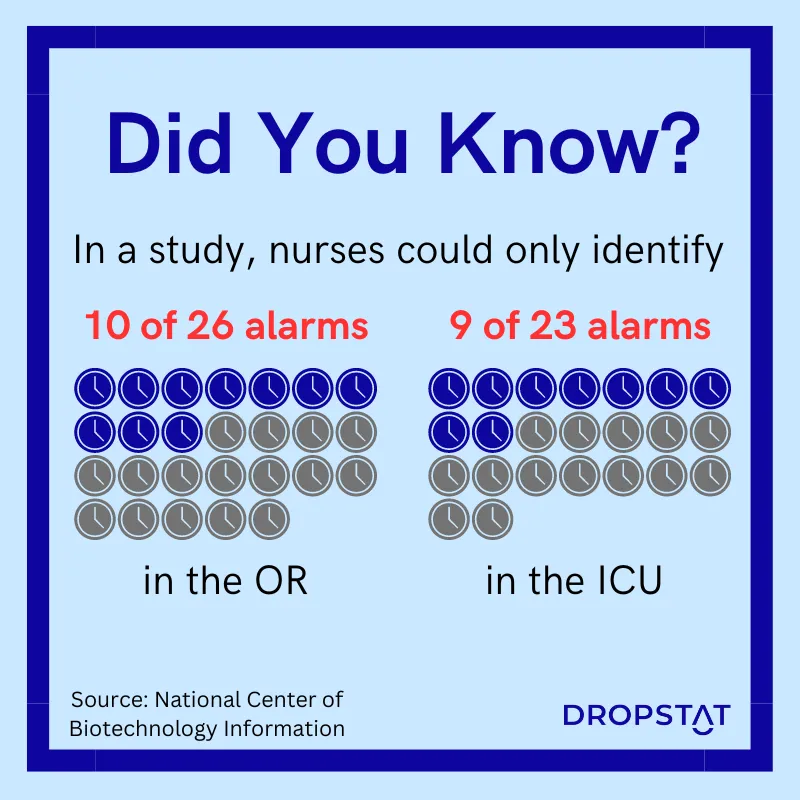
The Agency for Healthcare Research and Quality (AHRQ) points out that the greatest hazards in healthcare from alarm fatigue are cases of immediate danger to patient safety. This could occur if a nurse misses alarms for a fatal arrhythmia or a significant abnormality in a patient’s vitals. Alarm fatigue could happen if the patient’s heart rhythm monitor is known to give off false alarms. Lack of staff familiarity with alarm settings and which patients to monitor can be a risk factor for alarm fatigue; this can occur if the equipment is so advanced that nurses do not know how to use all the alarm settings on a monitor. Sown et al. studied nurses in an ICU setting. Up to 40% of the nurses reported not knowing 27 of their equipment’s functions and alarm settings.
How can alarm fatigue be measured?
Introducing a plan for alarm management in your facility begins with measuring alarm fatigue. Alarm fatigue is measurable mainly through nurse questionnaires for nurse leaders and critical care nurses. Wunderlich et al. recommend that nurses and physicians should be the target groups for clinical alarm questionnaires.







