What is cost containment in healthcare?
Cost containment in healthcare refers to a deliberate effort to control and reduce expenses associated with delivering medical services while not compromising the quality of patient care. Cost containment is a proactive response to the rising costs of equipment and medications and avoidable labor costs.
The Arizona Health Care Cost Containment System (AHCCCS) is a prime example of innovative and successful healthcare cost containment strategies, and it offers valuable insights to many other organizations for implementing effective cost-containment strategies. This healthcare system uses competition, choice, and patient cost sharing to successfully contain rising healthcare costs while improving patient care access. By leveraging their experience and exploring similar approaches, healthcare facility CEOs can find inspiration for their own cost-containment initiatives.
Why is cost containment important in healthcare?
Cost containment in healthcare is important since it ensures each healthcare facility’s financial stability and sustainability. Occasionally, hospitals that did not manage their health care spending correctly hit the headlines as they declare bankruptcy. CEOs can effectively allocate resources, streamline operations, and optimize financial outcomes by implementing cost-containment measures in healthcare spending.
Here are some areas in healthcare where cost containment strategies are crucial:
Cost containment in nursing
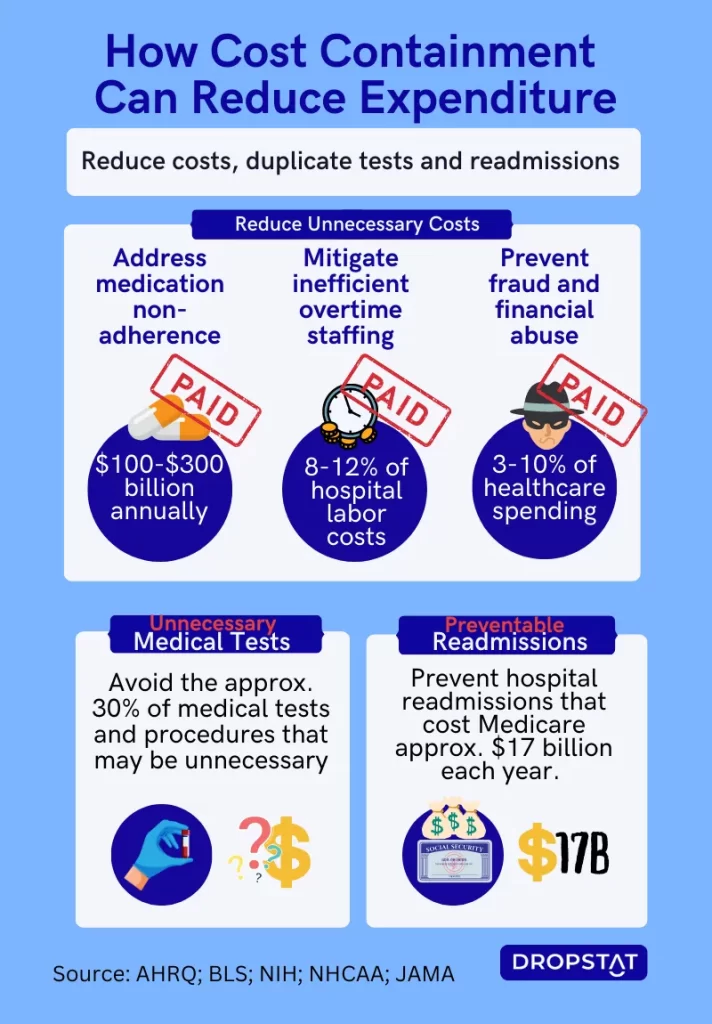
Cost containment in nursing means, practically, avoiding expenses such as nurse overtime. This alleviates the burden on overworked nurses while improving their job satisfaction and reducing burnout. This win-win approach also contributes to improved patient safety and quality of care.
Pharmaceutical costs
The rising prices of medications can place a considerable financial strain on healthcare organizations. Implementing cost containment measures such as formulary management, generic drug utilization, and negotiating favorable pricing contracts with pharmaceutical manufacturers can help mitigate healthcare costs. Promoting evidence-based prescribing practices and exploring therapeutic alternatives, such as acupuncture, physical therapy, and mindfulness techniques instead of or to augment expensive prescription drugs, can lead to cost savings.
Diagnostic testing and imaging
Effective cost-containment strategies use patient care programs that require only appropriate and necessary tests and imaging procedures.
Advancing and applying technology
Technological step-ups such as telemedicine and remote monitoring were created by necessity, but now these technologies enhance access to care and reduce the need for costly in-person diagnostic procedures. This demand-pull enables medical scientists to advance technology, and now the opportunities exist to apply these advances to real-life medical usage. Additionally, new technology, such as EHRs, allows facilities to pool medical knowledge, share resources, and share best practices.
Payment and reimbursement models
Shifting from fee-for-service to value-based care models incentivizes healthcare organizations to focus on delivering high-quality, cost-effective care. Insurance coverage goes further when healthcare spending is controlled.
Preventing fraud and waste
Implementing robust resource-monitoring systems, conducting regular audits, and promoting a culture of compliance can help identify and mitigate fraudulent activities.

What are the benefits of cost containment in healthcare?
Cost containment in healthcare offers significant benefits, including:
- Financial stability: Cost containment in healthcare ensures that financial resources are allocated efficiently and wisely. When healthcare organizations achieve financial stability, it allows for investment in other essential areas of healthcare, such as improving patient care, infrastructure enhancements, advanced technology, and quality improvement initiatives.
- Streamlining operations and eliminating wasteful practices: Cost containment leads to improved overall efficiency and productivity. By planning to reduce unnecessary healthcare costs, facilities are led to implement efficient staffing models, optimize workflow, and leverage technology.
- Nurse retention: Cost containment strategies in nursing directly impact the well-being and satisfaction of nurses. By implementing workload management systems, optimized staffing ratios, and efficient scheduling practices, healthcare organizations can alleviate the burden on nurses, reduce burnout, and enhance employee health. This, in turn, improves nurse retention rates and contributes to a more stable and satisfied workforce.
- Enhanced patient care: Cost containment strategies in hospitals often lead to improved patient outcomes. By optimizing resource allocation, implementing evidence-based practices, and leveraging technology, healthcare organizations can enhance patient safety, reduce medical errors, and deliver improved patient care.
- Sustainability and growth: Cost containment strategies lay the foundation for long-term sustainability and growth. Managing rising healthcare costs effectively fosters organizational growth and the ability to adapt to evolving healthcare demands.
- Competitive advantage: Healthcare organizations that successfully implement cost-containment strategies gain a competitive edge in the industry. By demonstrating efficient resource utilization and cost-effective operations, they attract patients, insurers, and healthcare partners. This positions the organization as a preferred choice and strengthens its reputation in the healthcare market.
Top 10 strategies for cost containment in healthcare:
Managers have a lot to gain from applying cost-containment strategies in healthcare. So let’s look at some top strategies.
- Supercharge your staff with a better staffing model: Implement optimal staffing models to ensure adequate coverage while minimizing unnecessary labor costs. Using workforce management systems, such as Dropstat, helps match staffing levels with patient demand to avoid overstaffing or avoidable nurse overtime.
- Advance patient throughput with streamlined operations: Identify inefficiencies in the workflow processes, and implement lean methodologies. These ideas can eliminate waste and improve operational efficiency. This includes reducing patient wait times, optimizing patient flow, and minimizing unnecessary administrative tasks.
- Reshape your facility’s healthcare acquisitions with strategic vendor management: Negotiate favorable contracts with vendors, suppliers, and service providers to secure competitive pricing and favorable terms. Regularly assess vendor performance and explore opportunities for cost savings through alternative sourcing.
- Implement proven innovations in technology integration: Take advantage of technology solutions to streamline operations, reduce paperwork, and identify cost-saving opportunities. For example, electronic health records (EHRs) and data analytics tools automate processes, improve accuracy, and enhance decision-making.
- Launch effective preventive care and chronic disease management: Prioritize preventive care initiatives and proactive management of chronic diseases through health services. By focusing on early intervention, education, and proactive treatment, healthcare organizations can reduce long-term costs associated with advanced and preventable conditions.
- Transform patient care with evidence-based medicine: Embrace evidence-based practices and clinical guidelines to ensure the appropriate and cost-effective use of healthcare resources. This approach helps reduce unnecessary care, tests, treatments, and hospital readmissions, leading to significant cost savings.
- Modify and enhance supply chain optimization: Implement cost-effectiveness in supply chain management, including centralized purchasing, bulk purchasing, and inventory control, to minimize healthcare costs associated with medical supplies, medications, and equipment.
- Develop and advance ports for telehealth and remote monitoring: Revamp the health system to adopt telehealth and remote monitoring technologies to provide cost-effective care options, reduce hospital readmissions, and improve access to care, particularly in rural or underserved areas.
- Amplify how you use health information exchange (HIE): Establish robust health information exchange systems to facilitate seamless sharing of patient information between healthcare providers. Interoperability in healthcare reduces duplicate testing, eliminates unnecessary procedures, and enhances care coordination.
- Revolutionize patient experience with continuous quality improvement: Foster a culture of continuous quality improvement by taking advantage of the CMS quality improvement programs, by actively engaging in quality assessment, performance measurement, and outcome analysis. By identifying areas for improvement, healthcare organizations can enhance patient outcomes while optimizing resource utilization.
A Dropstat case study of cost containment in healthcare
Let’s consider an example where an actual client of Dropstat, a multi-location healthcare facility, WeCare, implemented a more efficient healthcare staffing strategy with Dropstat, resulting in huge cost savings.
WeCare analyzed patient-demand patterns and implemented Dropstat’s workforce management system. The hospital chain wanted to reduce excessive labor costs and overtime hours.
As Dropstat moved into the picture, one of the WeCare facilities was spending an average of $31,000 monthly on bonuses and overtime costs. A second location was wasting $19,000 over 30 days in avoidable overtime. A little investigation revealed that a third location was paying out over $13,000 in monthly bonuses. Overtime in some facilities each year amounted to $124,800, $26,240, and $14,400.
With the implementation of optimized staffing practices, the facilities managed to reduce overtime significantly. Instead of allowing nurses to go into overtime, shifts were filled with other qualified staff.
WeCare applied the changes recommended by Dropstat in workforce management. The results were saving a huge $181,360 in bonuses and overtime!
A single WeCare facility achieved an average savings of $15,628.17 per month in overall staffing costs by introducing:
- Cost tagging on each staff member and any agency staff members
- Overtime tagging on every worker
- Early shift postings helped to avoid last-minute agency hiring
- Predictive analytics algorithms that helped the facility to learn from the past for the sake of the future staffing patterns
all through Dropstat’s AI-powered staffing app.
Over the course of a year, these amounts saved in each location amounted to substantial cost savings that could be redirected toward other critical areas of healthcare delivery or investments in facility improvements.
Calculations like these demonstrate the tangible and real-life impact of cost-containment strategies on the healthcare system and provide healthcare facility CEOs with concrete evidence of the financial benefits achieved through proactive cost management.

Which stakeholders should be involved in the cost containment process?
Cost containment in healthcare requires a collaborative effort that involves various stakeholders within the organization. When aiming to reduce existing healthcare costs and control future expenses, healthcare facility CEOs should engage the following key players in the cost-containment process:
- Leadership team and executives
The leadership team and executives play a vital role in driving the cost-containment initiatives. They set the vision, establish goals, and provide the necessary resources and support to implement effective strategies. The active involvement and commitment of leaders is crucial for fostering a culture of cost-consciousness and ensuring the success of comprehensive cost-containment strategies.
- Finance and accounting department
The finance and accounting department holds expertise in financial analysis, budgeting, and expense management. Their involvement is essential in assessing the current financial landscape, identifying cost-saving opportunities, and developing budgetary guidelines aligned with cost-containment objectives. They provide valuable insights into the financial implications of various strategies and help monitor and track cost-saving initiatives.
- Operations and process improvement teams
The operations and process improvement teams possess a deep understanding of the organization’s workflows, systems, and processes. Their involvement is crucial in identifying inefficiencies, streamlining operations, and eliminating wasteful practices. By conducting thorough process assessments, analyzing data, and implementing lean methodologies, these teams can identify areas where cost containment strategies can be most effective.
- Clinical and medical staff
The clinical and medical staff, including nurses, physicians, and other healthcare professionals, play a critical role in making cost containment more realistic. They possess valuable insights into clinical workflows, resource utilization, and patient care practices. Involving them in the cost containment process ensures that strategies are implemented without compromising patient safety or quality of care. They can provide input on evidence-based practices, appropriate resource allocation, and potential areas for improvement.
- Supply chain and procurement team
The supply chain and procurement team plays a significant role in cost containment, particularly in managing and optimizing the organization’s purchasing processes. They collaborate with vendors and negotiate contracts, and they must be part of implementing the strategies. Their involvement in the cost containment process is crucial for identifying cost-saving opportunities, implementing inventory management systems, and fostering strategic supplier relationships.
- Information technology (IT) department
The IT department is instrumental in implementing technology solutions that support cost-containment initiatives. They can assist in automating processes, implementing electronic health records (EHRs), and integrating systems for better data analysis and decision-making. Expertise in IT helps leverage technology to streamline operations, reduce administrative costs, and enhance overall efficiency.
A successful cost-containment process in healthcare requires the involvement and collaboration of multiple stakeholders. All stakeholders contribute their unique expertise to implement the strategies and maximize the impact of cost-containment initiatives.
Barriers to an effective cost-containment strategy
While cost containment in healthcare is crucial for maintaining an organization’s good reputation and efficient healthcare management, several barriers can impede the implementation of effective strategies. These include resistance to change, for which managers can help break down barriers with effective change management; having limited data and analytics; having a complex regulatory landscape; having fragmented systems and communication; and having a lack of employee engagement.
Balancing cost and quality
Another barrier that facility managers often have to overcome is striking the right balance between cost containment and high-quality patient care, which can be challenging. Reducing staffing levels, for example, as a cost-saving measure in healthcare is not the solution. Instead, implementing evidence-based practices and continuous quality improvement programs can help address this barrier effectively.
How Dropstat can help healthcare facility managers with cost containment
Dropstat, an AI scheduling app, helps managers effectively cut staffing costs by reducing nurse overtime and bonuses and hiring expensive agency staff. Dropstat allows staff schedulers to control staffing patterns and fill shifts effectively. Schedulers can fill shifts up to 2 months in advance and fill understaffed shifts with internal staffing resources. Schedulers can seamlessly selectively send out open shift requests based on the nurses’ qualification levels and cost tagging of staff. This ensures that the facility does not overpay for overqualified staff or for nurses going into overtime.
Dropstat also identifies recurring staffing shortages and advises the facility where to hire a permanent staff member instead of resorting to expensive agency staff.
Schedule a demo with Dropstat to find out more about Dropstat’s powerful staff scheduling app and how it can become your next cost containment initiative.







