What Causes Nurse Burnout?
There are several factors that can cause burnout in nurses. These factors are especially likely to lead to burnout when more than one is present:
- Long shifts
- Lack of sleep
- High-stress environments
- Lack of support
- Emotional burdens as a result of patient care
- Low staffing
- Inadequate shift breaks
- Heavy workloads
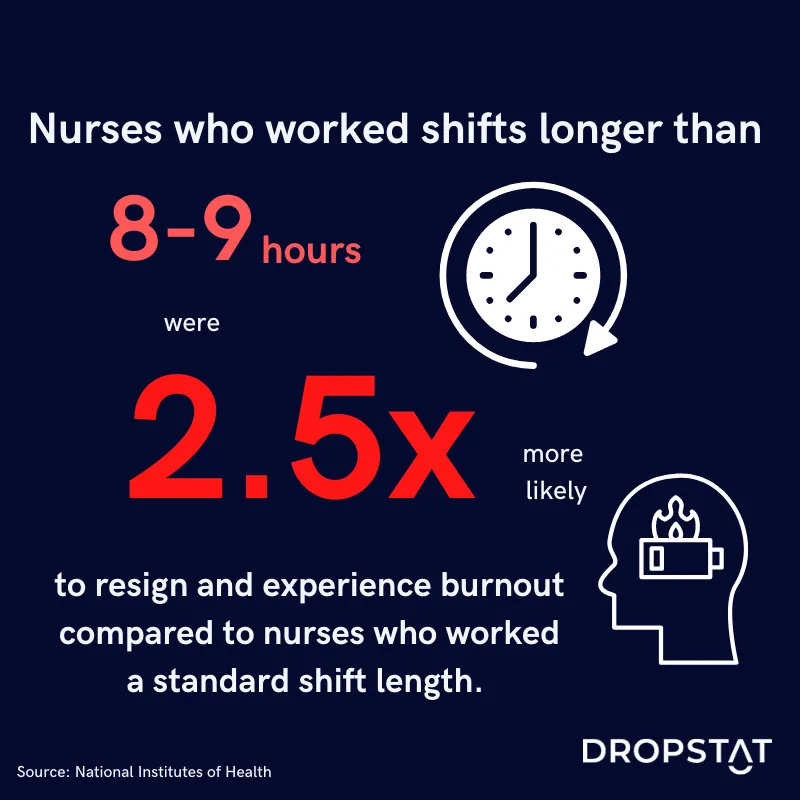
Longer shifts
According to research from the National Institutes of Health, nurses who worked shifts longer than 8-9 hours were up to 2.5 times as likely to resign and experience burnout and job dissatisfaction compared to nurses who worked a standard shift length.
Not enough sleep
Tired nurses are at high risk for burnout. When facilities rely heavily on nurses working overtime and/or back-to-back shifts, the burnout risk increases significantly. Nurses need enough sleep between shifts to regain their physical and emotional energy. If they don’t get adequate sleep, they clock in to their next shift already feeling depleted. This perpetuates a constant cycle of physical and emotional exhaustion– a major symptom of burnout.
High-stress environments
Nursing is a fast-paced job that comes with high-stress levels. Nurses routinely encounter stress factors, including exposure to hazardous drugs, infectious diseases, unpredictable schedules, and demanding physical work. Nurses experiencing high-stress levels at work for prolonged periods of time are far more likely to report job dissatisfaction.
Lack of support
A 2021 study focusing on the COVID-19 pandemic found that a lack of social support contributed heavily to nurse burnout during COVID. Healthcare workers who did not receive appropriate social support were at greater risk for developing psychological issues. A strong support network allows nurses to process negative emotions, reduces feelings of isolation, and reduces the risk of burnout.
Emotional burden from patient care
Nursing takes compassion, but nurses emotionally invested in patient care without time to recuperate can experience emotional exhaustion. A 2021 study indicates that nurses who cared for critical patients or patients that had passed away experienced strong emotions of helplessness, compassion, sadness, and depression. When nurses were by a patient’s side as they experienced death, their levels of anxiety and depression significantly increased. These emotional burdens contribute to burnout among nurses.
Low staffing
Insufficient staffing ratios significantly predict nurses’ plans to resign from their jobs. When healthcare facilities are understaffed, nurses are overwhelmed with more patients than they can care for effectively and safely. An impossible workload spikes stress levels and results in nurses performing poorly consistently. Many nurses, frustrated by the vicious cycle of inadequate staffing, seriously consider quitting their jobs.
Lack of adequate shift breaks
Constantly running from one patient to the next is tiring, to say the least. Nurses who spend their entire shift caring for patients without a break can quickly develop severe fatigue. Many nurses report skipping their lunch breaks and even foregoing bathroom breaks to deliver patient care. Nurses are people, not machines, and if nurses don’t take the breaks they need, they can burn out very quickly.
Heavy workloads
When nurses are assigned heavier workloads than recommended, both quality of patient care and patient safety is put in jeopardy. Nurses with heavy patient workloads made more errors while providing care, experienced decreased job satisfaction, and decreased overall health – all of which increase potential burnout.
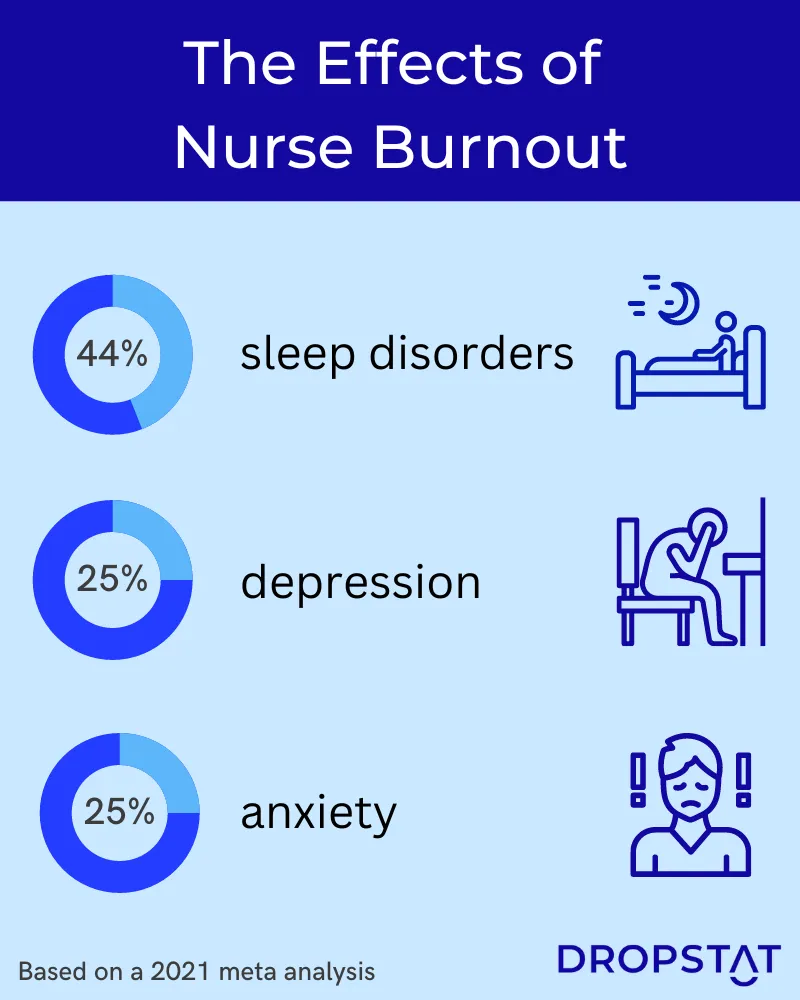
Nurse Burnout Symptoms
There are numerous ways that individuals exhibit physical, emotional, and behavioral signs of burnout.
Here are some physical indications of burnout to look for:
- Disruptions in normal sleep patterns and appetite
- Anxiety
- Exhaustion
- Headaches
Typical emotional indicators of burnout include:
- Detachment
- Lack of motivation
- Lack of empathy
- Self-doubt
Prominent behavioral displays of burnout include:
- Frustration
- Impatience
- Procrastination
- Poor judgment calls
How to Prevent Nurse Burnout
While it may seem like these conditions are simply part of the nursing field today, there are clear steps that healthcare facility management can take to prevent nursing burnout. Facilities need to prioritize burnout prevention to ensure effective and efficient patient care as well as the well-being of their staff. Some tips on how to manage employee burnout include:
- Ensuring adequate time for breaks
- Establishing shorter shifts that do not exceed 9 hours
- Scheduling shifts in advance (to reduce nurses working sporadic shifts)
- Providing additional support to nurses
- Acknowledging employees’ hard work
- Instituting safer staff-patient ratios
More breaks
When nurses have mandatory breaks in their schedules, they are required to spend some time caring for themselves and recuperating their physical and emotional energy. This scheduled “me-time” enables them to function optimally and deliver patient care to the best of their abilities. Nurses who have a chance to catch their breath make less mistakes in patient care, which translates to increased patient safety and overall higher profitability for the facility. Institute a break accountability system, such as a separate time tracking system for taking shift breaks; add an additional short mandatory break to nurses’ schedules or try increasing the current break time by even five minutes. Staff will feel more satisfied with their jobs and less fatigued, dropping burnout and turnover rates in your facility.
Reducing shift length and overtime
Like sufficient breaks, shifts that exceed nine hours contribute to fatigue, job dissatisfaction, and ultimately, burnout. By reducing excessive shift length and overtime, nurses will be able to create a healthier work-life balance which will allow them to maintain healthy sleep patterns and recover from the emotional burdens of each shift.
Scheduling shifts in advance
In practice, one effective method to reduce overtime is to post shifts well in advance. By indicating required shifts as early as possible, nurses have the opportunity to prepare for their hours and create schedules that align well with their personal life. Conveying scheduling needs to staff plays a crucial role in decreasing burnout and turnover. Furthermore, it allows management to identify which shifts require additional staffing support to reduce nurses’ workload and overtime.
Providing additional nursing support
Nurses encounter emotionally challenging situations daily in their work, such as witnessing patient mortality and caring for patients who may be verbally abusive. These scenarios are emotionally cumbersome and leave nurses feeling drained and fatigued. By providing a system of social support either through other nurses or support groups, employees can process intense emotions in a healthy way, and compartmentalize their work and personal life, allowing them to rest and rejuvenate.
Appreciating employees
A small gesture of appreciation for nurses’ hard work goes a long way. A “nurse of the week” bulletin board, a thank you card, or a $5 gift voucher for the coffee shop across the street all communicate to your staff that you recognize their hard work and appreciate them. Nurses who feel noticed and heard have greater job satisfaction and a sense of mission, which keeps burnout at bay.

Instituting safer staff-patient ratios
When healthcare facilities have reliable and safe staffing ratios, workloads for individual nurses decrease. Typically, a staff-patient ratio of 1:4 is a safe staffing level, although these ratios depend on the unit. Sticking to safe staffing protocols prevents excessive workloads for individual nurses in addition to feeling burnt out and overwhelmed on the job.
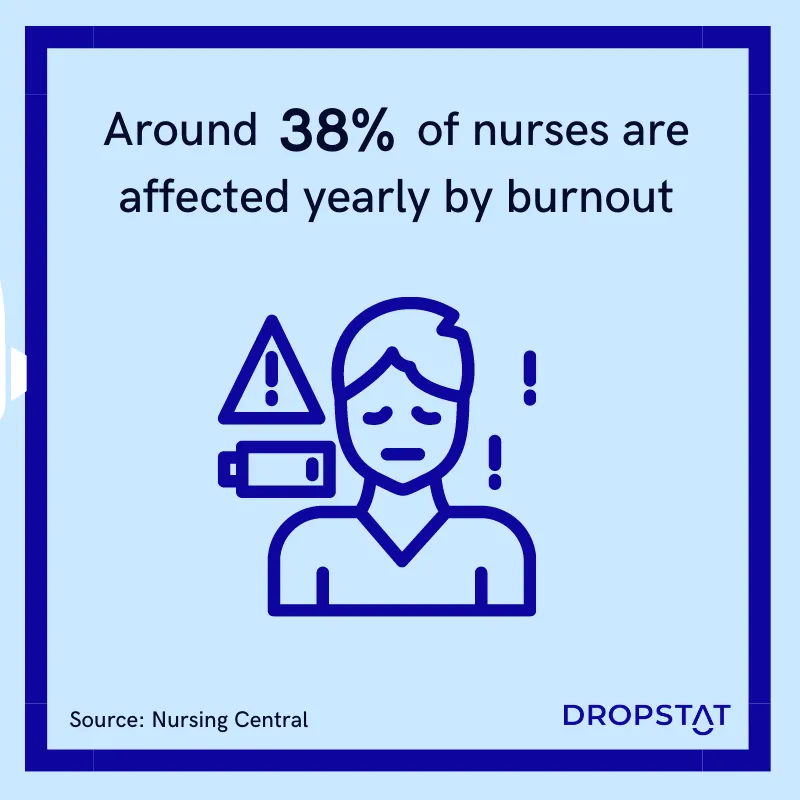
Nurse burnout statistics:
A survey conducted by Nursing Central revealed that:
- As of July 2021, 95% of nurses experienced current or previous feelings of burnout
- 91% of nurses were thinking about resigning or were looking into other careers
- 44% of nurses expressed that management ignored their issues after they had let the administration know
- 27% of nurses revealed that they did not feel secure in taking their issues to those in charge.
- Around 38% of nurses yearly are affected by burnout
How can Dropstat help with nurse burnout?
Dropstat’s systems work to effectively alleviate the nursing shortage and combat nurse burnout. Dropstat’s system flags nurses going into overtime by accepting an additional shift, so facilities can more easily limit nurse overtime. Allowing nurses to fully recuperate between shifts prevents them from becoming overworked and burnt out.
Dropstat encourages schedulers to provide ample lead time to fill shifts in advance. This eases the stress of filling required shifts at the last minute and allows nurses to plan their schedules weeks in advance, reducing work-related stress.
Dropstat’s shift planning software helps mitigate burnout in nurses and its costly repercussions for nurses, management, and patients. Is your facility ready to halt nurse burnout in its tracks? Schedule a demo to see how Dropstat can help your nurse burnout rate.






