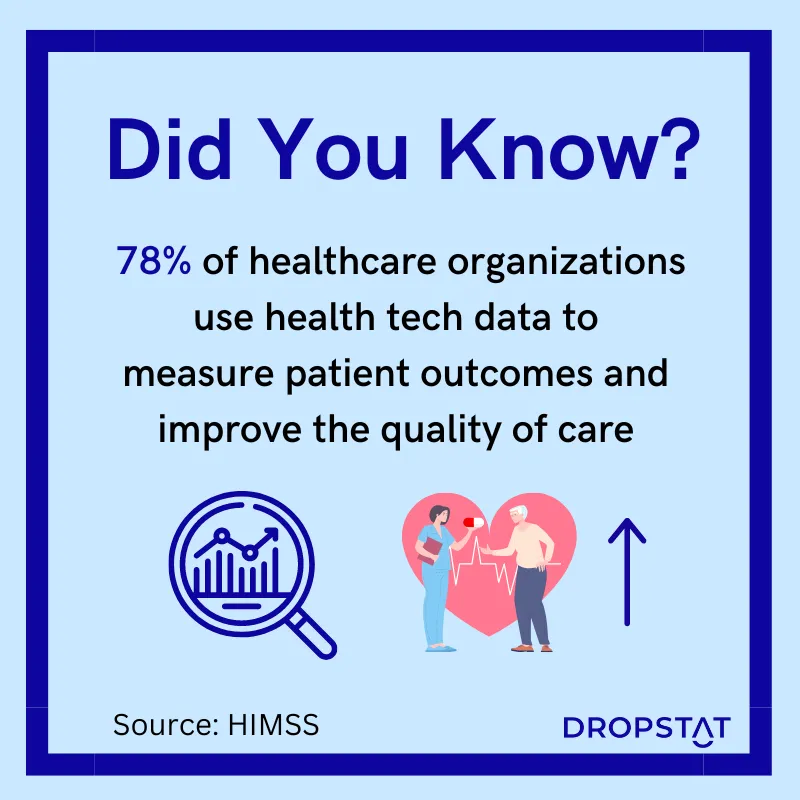
The current healthcare environment and its complexities demand a focus on quality improvement to promote more patient-centered and value-based care delivery. This emphasis on measuring healthcare performance ultimately leads to more positive patient outcomes and reduced healthcare costs. Concerning healthcare, some methods commonly used to measure performance include key performance indicators and quality metrics, which help evaluate processes within your healthcare organization.
Why are KPIs in healthcare important?
The primary purpose of KPIs and quality metrics in healthcare is to gain insight into the outcomes of your healthcare processes, allowing for meaningful measures of your institution’s goals. Understanding the logistics of your operations and assessing your practices enables your facility to improve transparency across all aspects of the care continuum, increasing patient experience and outcomes and reducing costs. Furthermore, tracking KPIs and clinical outcomes also helps quantify healthcare processes and improve employee satisfaction and retention rates. Healthcare organizations can not implement targeted solutions without KPIs and specific quality metrics.
3 key features of effective quality measures in healthcare
Structural Measures
One vital aspect of successful healthcare delivery includes the structural components of health systems. These features allow healthcare organizations to determine care quality through elements such as staffing ratios, sufficient medical supplies and equipment, and adequate clinical skills among the care team. Analyzing structural measures enables healthcare providers and institutions to determine their ability to deliver high-quality care based on patient volume and needs.
Process Measures
Similarly, process measures in healthcare help assess whether workforce practices result in better patient outcomes. Typically, process indicators align with clinical and other regulatory standards, which helps promote patient-centered care. Examples of process measures include establishing practices to ensure safe nurse-to-patient ratios and reduce employee burnout by decreasing overtime shifts to provide greater attention to each patient’s needs. This leads to better safety measures and reduced mortality throughout each unit.
Outcome Measures
Lastly, patient care can be quickly evaluated through health outcomes which indicate attention to varying patient needs and potential oversights in staffing strategies. One outcome measure commonly tied to patient safety includes hospital-acquired infections, which may result from inadequate staffing techniques. However, tracking health outcomes provides concrete quality metrics which allow a healthcare facility to adjust its structure and process to support better clinical outcomes, increased patient and employee satisfaction, and cost reduction.
How can healthcare KPIs improve safe staffing?
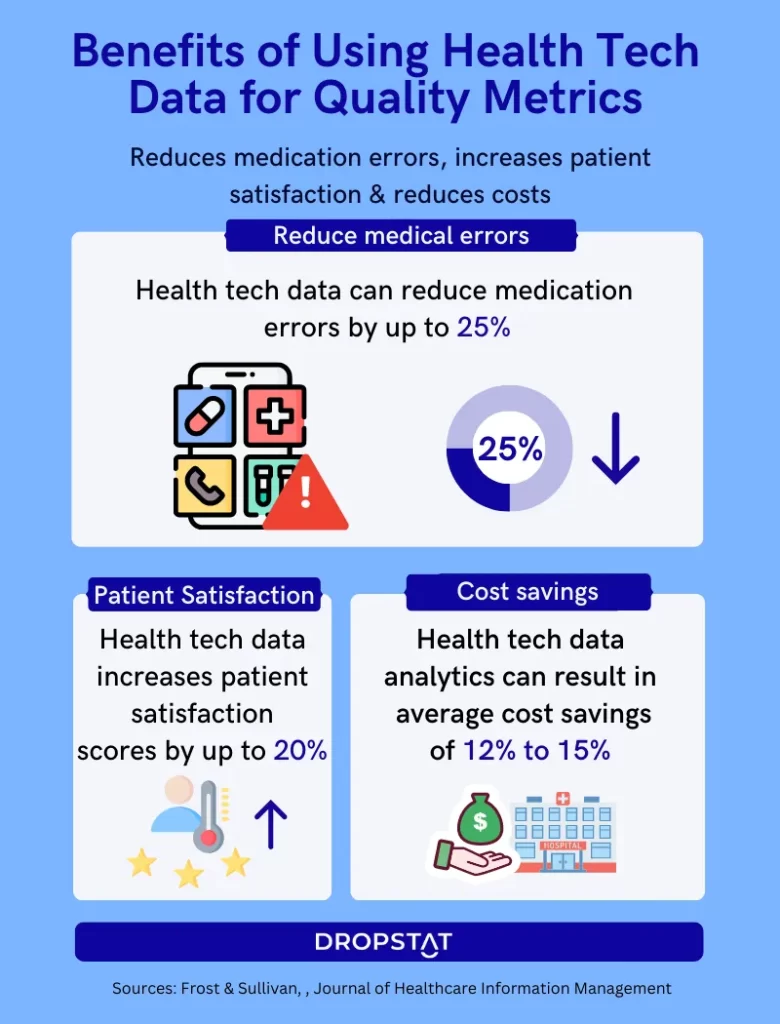
Healthcare KPIs can also improve staffing strategies by tracking metrics such as understaffed, overstaffed, and overtime shifts. This knowledge allows schedulers to identify insufficiently staffed departments, units, and shifts, empowering them to adjust their staff schedules to best support patient volume and meet HPPD requirements. Furthermore, these adjustments can help reduce medication errors and improper clinical practices by providing proper attention to each patient, thereby reducing the hospital readmission rate and unnecessary costs.
Challenges of quality metrics and KPIs in healthcare
While KPIs can provide your facility with specific and concrete information, it may be difficult to create change with the information provided. Additionally, other common challenges with KPIs include tracking too many quality metrics, changing processes based on short-term measures, and collecting data on KPIs that do not accurately represent the strategic planning goals.
How do quality metrics in healthcare advance strategic planning initiatives?
When healthcare organizations utilize their quality metrics to develop institutional objectives, they can set more achievable and long-lasting goals. Relying on data from quality metrics to define short-term and long-term goals enables your facility to determine which aspects require the most attention to reach their optimal workflows.
Dropstat’s success chart KPIs
The ability to track facility success allows schedulers and administrators to focus their efforts on the main challenges within their facility. Therefore, Dropstat equips each facility with the ability to track vital KPIs such as:
- open shifts
- filled shifts
- overtime
- agency
- shift bonus
- active staff
In the success chart below, we can see that for the month shown, this facility had 11 unfilled shifts that were sent out, which still required staff. Additionally, this facility used 0 hours of agency staff for the month, which did not exceed their goal of 200 hours or less. However, if a facility had used a significant number of agency-staffed hours, they could reduce the amount of agency by having a greater percentage of filled shifts and active staff who could proactively fill these shifts instead. This would mitigate the need for agency nurses, reduce spending on staffing, and ensure more safely staffed units.
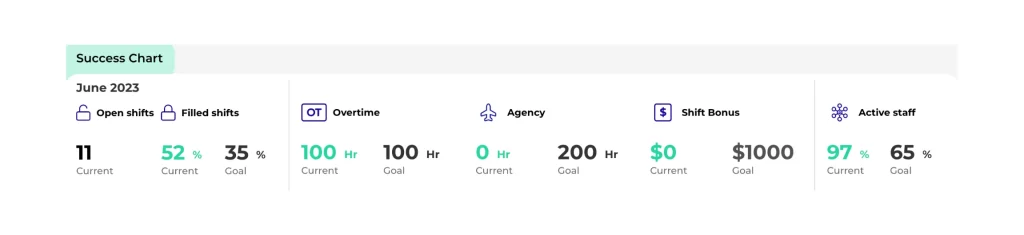
How does Dropstat track KPIs and implement strategies to improve them?
This success chart feature supports data-driven decisions regarding current and future staffing requirements. It also helps minimize expensive staffing methods such as overtime and agency usage that lead to higher staffing costs. Ultimately, the insight into specific staffing metrics, including how many overtime hours your staff is partaking in and working on effective ways to reduce this, helps reduce clinical errors made by fatigued nurses and prevent unsafe clinical environments, which ensures greater patient safety. By providing your scheduling team with quantitative data, you can create effective staffing and patient-centered practices that work to support both employee and patient satisfaction.
Schedule a demo with Dropstat to better understand your staffing KPIs and implement effective staffing strategies for optimum care and reduced healthcare costs.







