What is patient flow in healthcare?
The classic definition of patient flow is the movement of patients through various stages of healthcare delivery. Patient flow is a journey that starts from the patient’s point of entry. It continues until patient discharge or patient transfer to follow-up care. Patient flow refers to the entire patient journey, including the registration, triage, diagnosis, treatment, and discharge processes.
Effective patient flow management involves streamlining these processes to minimize bottlenecks, reduce waiting times, and ensure smooth transitions between departments while maintaining the highest patient safety and care standards.
Patient flow is also known as patient throughput, which refers to the rate at which patients move through the healthcare system, from admission to discharge or transfer. The patient throughput rate reflects the efficiency of the patient flow process.
Why is patient flow important?
There are several reasons why patient flow is important in improving healthcare. Patient flow principles can help healthcare organizations improve their efficiency in order to survive the demanding economic environment created today by healthcare regulatory bodies, funding institutions, and an aging population. Here are some points that show why patient flow is important.
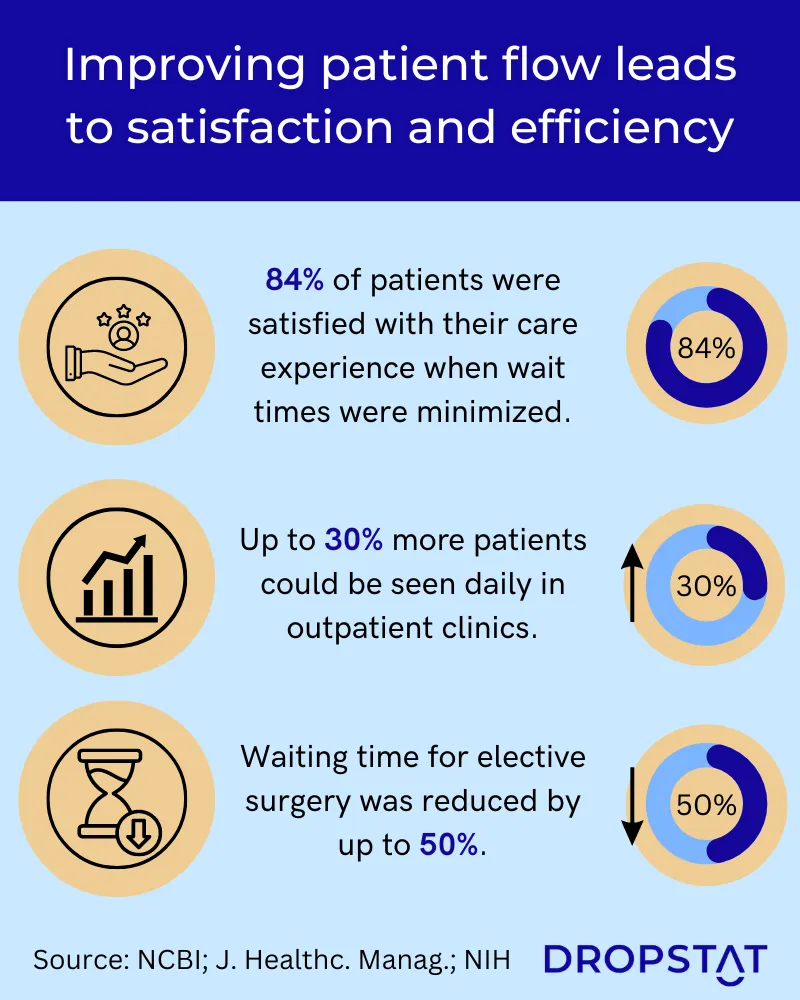
1. Enhanced patient experience
Efficient patient flow directly translates into improved patient experience. Long waiting times and delays can lead to frustration, anxiety, and dissatisfaction among patients and their families. Healthcare facilities can minimize waiting periods, enhance communication, and provide patients with a seamless and comfortable care experience. This, in turn, boosts patient satisfaction, builds trust, and fosters a positive public image, benefiting both the facility’s reputation and patient retention.
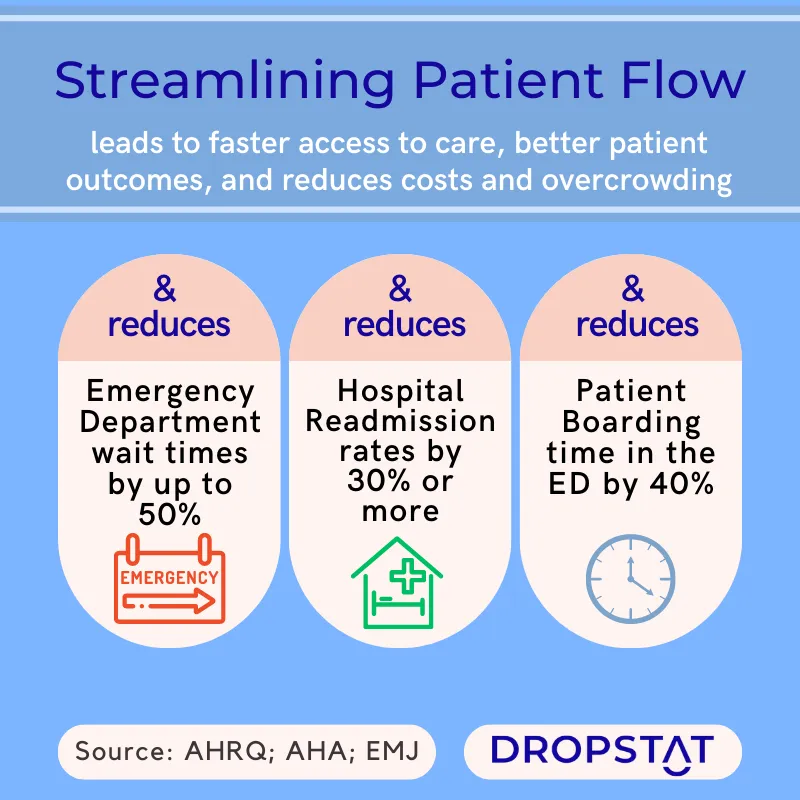
2. Timely access to care
Effective patient flow management ensures timely access to care for patients. Delays at any stage of the patient journey can lead to adverse health outcomes, prolonged suffering, and potential complications. Healthcare facilities can prioritize patients based on urgency, ensuring timely intervention and improving patient outcomes.
Swift access to care is particularly crucial for emergency departments, where efficient patient flow can save lives. “Boarding” happens when patients wait in the ED for a bed to become available in inpatient units. An emergency medicine physician, Dr. Peter Viccellio, M.D., caused boarding to be “sharply reduced” since 2001 when he introduced sounder procedures for improving hospital-wide patient flow problems, especially in the ED. Many facilities use Viccellio’s patient flow principles when determining how to improve patient flow in hospitals.
3. Workflow efficiency
Patient flow management promotes streamlined workflow and collaboration among healthcare professionals. Healthcare facilities must ensure seamless information exchange and communication between departments. A coordinated approach between patient flow team members reduces errors, improves care coordination, and enhances the overall efficiency of healthcare teams.
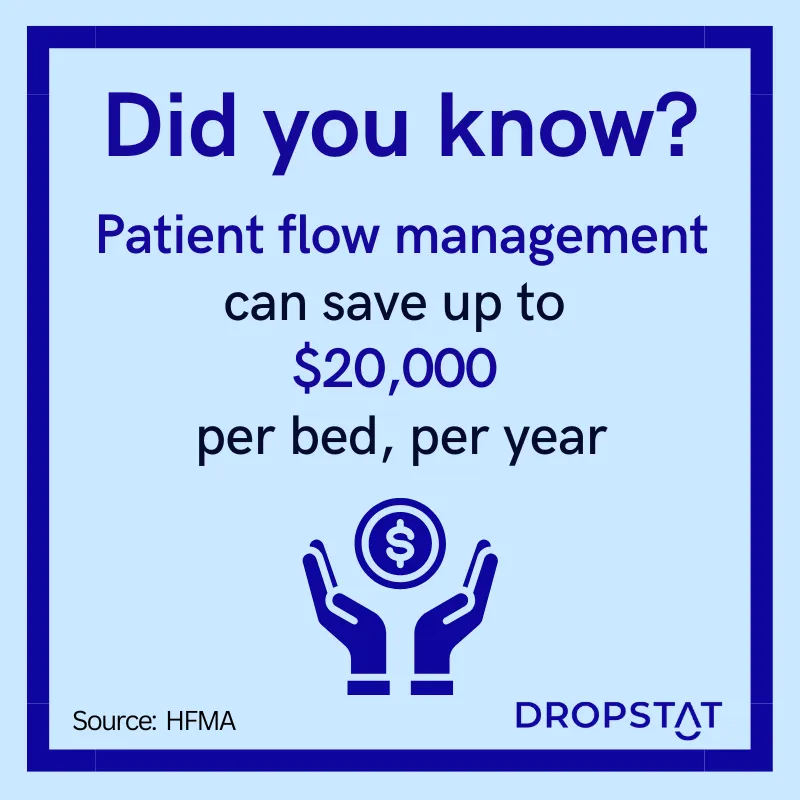
4. Financial viability
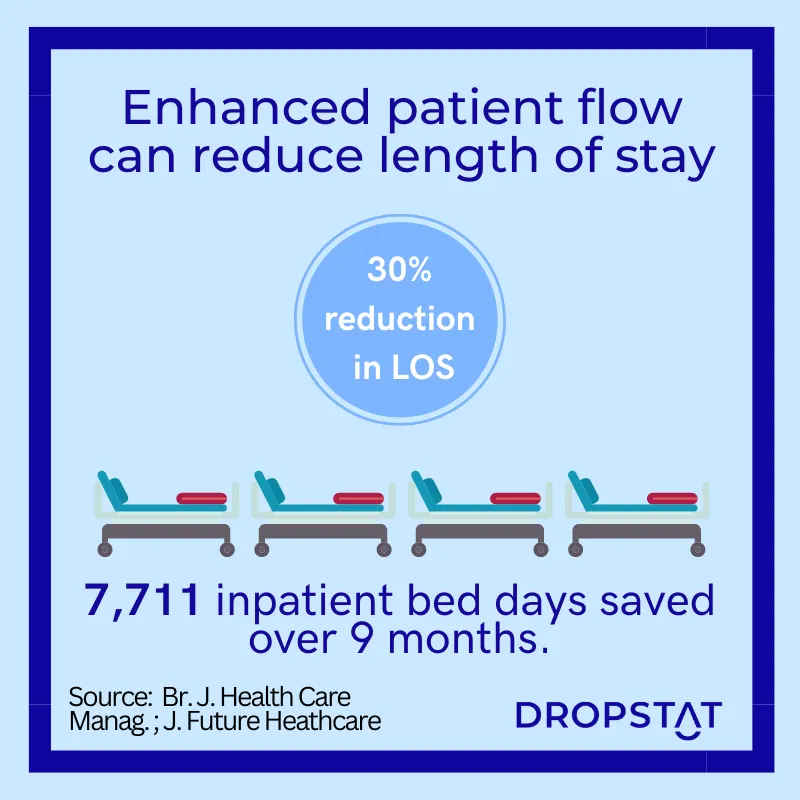
Optimizing patient flow contributes to financial sustainability. By improving patient flow, healthcare providers can accommodate more patients within the same resources, thus increasing revenue generation. Moreover, efficient patient throughput reduces the length of stay (LOS), enabling facilities to manage patient volumes effectively and optimize bed utilization. These factors collectively contribute to improved financial performance and cost containment in healthcare.
One hospital found that improving their patient flow reduced procedure turnaround time from 31.6 hours to 15.3 hours, and average LOS was reduced by over 2 days.
What factors affect patient flow management?
Patient flow management requires a comprehensive understanding of the factors influencing the entire patient flow process. Here are some of the main factors that affect patient flow management to help healthcare leaders identify areas of improvement and implement patient flow solutions that will enhance the quality of care and reduce facility costs.
Workflow design and process standardization
The design and consistency of workflow processes within any healthcare facility are crucial to patient flow optimization. Healthcare facilities can establish clear protocols and minimize variation in processes between different departments for consistent delivery of care. This approach promotes smooth transitions between departments, reduces confusion, and enhances overall workflow efficiency.
Resource allocation and capacity management
When assessing patient volume, acuity levels, and available resources, healthcare facilities must make informed decisions about staffing levels, equipment availability, and room utilization. Proper planning and resource allocation prevent overcrowding, reduce waiting times, and enable timely delivery of care to patients.
Care coordination and communication
Efficient patient flow relies on effective care collaboration and the presentation of patient information. Timely exchange of patient data, test results, and treatment plans is essential for a smooth transition between different stages of patient care. Using electronic patient records and real-time communication enhances patient throughput.
Patient prioritization
Appropriate assessment of patient status and priority of care are critical to managing patient flow effectively. Healthcare facilities can ensure that resources are allocated first to those in greatest need. Regularly reassessing patient status contributes to optimal interventions. Waiting room nurses were observed to not only calm patients in the emergency department and contribute to patient safety but also facilitate the flow of patients out of the waiting room mainly by reassessing and detecting deterioration in the patient’s condition.
Bottleneck identification and process improvement
Regular analysis of patient flow data helps identify patient flow bottlenecks and inefficiencies within the system. Through patient flow analysis, healthcare facility CEOs can pinpoint specific stages or departments where delays occur. Then, by implementing targeted process improvements, department managers can eliminate bottlenecks and enhance patient flow.
Who is on the patient throughput team?
The success of patient flow management relies on a collaborative effort involving various healthcare professionals working together as a dedicated patient throughput team. The team comprises individuals from different disciplines who are crucial in optimizing the patient flow management system and ensuring efficient care delivery.
- Healthcare administrators provide strategic supervision, support, and resources for patient flow initiatives.
- Nursing and clinical staff monitor patients, coordinate treatments, and ensure smooth transitions between different stages of care.
- Physicians and specialists share their expertise and timely decision-making for managing patient acuity levels and prioritizing care.
- Support staff, including medical assistants, technicians, and ancillary service providers. They facilitate patient registration, coordinate diagnostic tests, and ensure the availability of necessary equipment.
- Care coordinators facilitate communication between healthcare providers, arrange follow-up appointments, and help streamline the discharge planning process. Their support is noticeable, particularly for patients with complex needs.
- Institute for Healthcare Improvement (IHI) advisors – in some cases, healthcare facilities may engage IHI advisors who specialize in healthcare improvement methodologies. These advisors provide expert guidance, data analysis, and implementation support to optimize patient flow, reduce crowding in emergency departments, and enhance overall healthcare delivery.
Additionally, as an outcome of the specific needs of the healthcare facility, the patient flow team may also involve other stakeholders, such as behavioral health providers, social workers, and community outreach professionals, who contribute their expertise to address unique patient flow challenges.
10 ways to improve patient flow in healthcare
Here are 10 effective strategies to help healthcare managers succeed in improving patient throughput, increasing patient satisfaction and experience, providing better quality care, and reducing healthcare costs.
1. Streamline registration and check-in processes
Simplify and automate registration and check-in procedures to minimize patient wait times. Implement electronic check-in systems, pre-registration options, and digital forms to expedite the process and reduce paperwork.
2. Optimize appointment scheduling
Efficient appointment scheduling is crucial for patient flow. Implement advanced, accessible, online appointment-scheduling systems that consider patient needs, provider availability, and resource allocation to minimize gaps due to patient cancellations and avoid overbooking.
3. Enhance communication and information exchange
Improve care coordination and information exchange between healthcare teams to streamline patient flow. Utilize EHRs and real-time communication platforms to ensure efficient instant access to patient information, test results, and treatment plans.
4. Implement proven triage and prioritization systems
Apply standardized, proven triage protocols to assess patient acuity levels and prioritize treatment accordingly quickly. Obligate all staff to take triage training programs to ensure consistent and accurate patient assessment.
5. Optimize resource allocation
Regularly assess patient volumes, acuity levels, and resource availability to optimize resource allocation. Utilize patient flow analysis and electronic equipment tracking to identify areas where resources and medical supplies cannot keep up with demand and make data-driven decisions for effective distribution.
6. Implement lean process improvement strategies
Practice continuous improvement by analyzing patient flow goals, identifying patient bottlenecks, and implementing targeted improvements to boost patient throughput. Use a staff attendance and tracking app such as Dropstat to identify shifts that are understaffed (leading to longer waiting times, reduced quality of care, and higher levels of medical errors, readmissions, and morbidity). Dropstat enables continuous improvement in staffing and allows facilities to meet required staffing ratios in a way that creates the most value for a facility.
7. Enhance discharge planning and care transitions
Expedite patient discharge with automated systems and facilitate smooth care transitions. Provide patients with clear instructions and a personalized discharge plan to ensure the smooth transition of a patient from the facility and offer several options for post-discharge medical support to avoid delays at discharge.
8. Utilize technology solutions
Leverage technology to optimize patient flow. Implement automated patient tracking systems, electronic prescribing, and digital documentation to enhance workflow efficiency and reduce manual errors.
9. Promote staff training and collaboration
Invest in staff training programs to enhance staff skills and knowledge in patient flow management for achieving hospital-wide patient flow. Encouraging inter-departmental communication and teamwork will encourage efficiency in the patient flow system. This includes non-clinical staff such as transportation, housekeeping, and staff carrying out administrative tasks. Their speed and efficiency have a significant impact too.
10. Continuously monitor and evaluate patient flow
Regularly monitor patient flow metrics and conduct performance evaluations to identify areas for improvement. Use patient flow analysis tools to track key performance indicators and implement appropriate patient flow solutions.
By implementing these strategies, healthcare facilities can boost patient flow in clinics and hospitals, improve patient throughput, and achieve optimal resource utilization.
How Dropstat’s features can help optimize patient flow
Dropstat’s AI-powered staffing app supports patient flow optimization by making sure that each shift is fully staffed and the right HPPD ratios are always maintained. This ensures that patients are given the optimum patient care, which speeds up the recovery process and helps improve hospital-wide patient flow.
Ensuring that HPPD compliance is maintained also benefits healthcare staff members, allowing them to work most efficiently. The staff scheduler is able to see if all staff are present in their shifts. With all necessary staff present, the workload will be shared fairly and helps nurses to contribute their best to the patient flow system.
Schedule a demo to discover how you can optimize patient flow and see how advanced data analytics can improve facility efficiency.







