The importance of revenue cycle management – healthcare (RCM)
Gathering clear insights into your facility’s revenue cycle management process is the key you need to detect weaknesses in your operations which will have profound effects on patient experience and satisfaction. The most significant impact of RCM includes:
- increased financial stability
- improved patient satisfaction ratings
- greater operational efficiency
RCM is the tool that healthcare facilities need to ensure that reimbursements are both prompt and accurate to reduce potential claims denials and undetected loss of revenue. This leads to improved financial stability while prioritizing astounding revenue cycle performance.
Additionally, when healthcare providers implement efficient revenue cycle management healthcare strategies, they experience a monumental reduction in medical billing errors, such as improper coding. Not only do fewer billing errors lead to communicating and verifying patient financial responsibility in a timely manner, but it also increases patient satisfaction and loyalty to your facility!
7 Steps in The Revenue Cycle Management Process
Each stage of the revenue cycle management process plays a key part in collecting revenue and ensuring industry compliance.
1. Preregistration: This is the initial step in the RCM process, which includes gathering patient insurance and demographic information. This step ensures that patients are aware of their financial responsibilities, empowering them to feel confident in the facility’s transparency and communication methods.
2. Registration: The mission of registration, which is the second step in the RCM process, involves confirming patient information, such as co-payments, contact information, and insurance, in order to avoid future collections challenges.
3. Charge capture: This step leads the way in translating correct medical codes into charges. These charges are then submitted to patients’ insurance providers for reimbursement to ensure that providers are accurately compensated.
4. Claims Submission: The fourth step in revenue cycle management includes communicating with insurance providers regarding the recorded diagnosis codes. This process requires great precision to ensure that claims are sent without errors.
5. Remittance processing: This stage takes us through the journey of insurance coverage by explaining the coverage for the medical services that were provided or an explanation of benefits about payment for the services. Fee schedules, which are the amounts charged by providers and paid by insurance companies, are also an integral part of the remittance process.
6. Insurance follow-up: This uncovers the amount that has been paid by insurance, as well as the remaining amount that the patient is expected to cover. Reviewing the report of accounts receivable (A/R) allows you to lift the fog from patient collections. This helps you easily determine the amounts that have not yet been collected from patient payments or from insurance. Insurance follow-ups equip you to determine whether there may be an issue with the specific health insurance companies to investigate further.
7. Collections: The final touch for the revenue cycle management healthcare process, collections, requires that patient statements are sent out in a timely manner and that staff members prioritize collections when patients are in the office. This prevents bad debt and helps you improve the efficiency of the revenue cycle management processes. Ultimately, this increases value-based care and reduces administrative costs associated with revenue cycle errors, maintaining a strong and efficient RCM process.

Effective Revenue Cycle Management Practices
Considering that revenue cycle management utilizes many different steps, implementing methods to simplify and maximize its benefits to ensure that payments are received on time can take your facility to the next level.
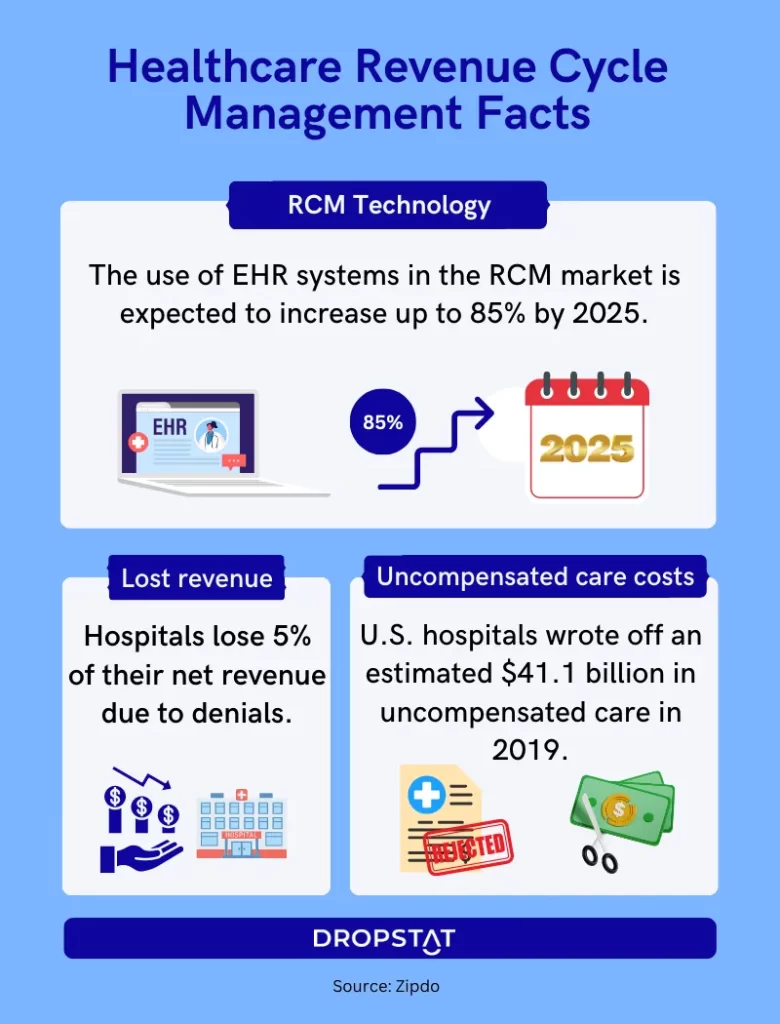
Integrate technology into the RCM processes
Some techniques that will completely transform your RCM procedures include increasing the use of technology in financial processing, including healthcare information technology, and taking advantage of electronic medical records, which reduces the administrative burden on your staff. In addition, using AI to automate RCM processes such as registration and preregistration, improve the patient experience, and streamline processes for authorization and patient insurance information verification, are all processes that healthcare organizations can carry out to alter the course of your facility’s revenue.
Seamlessly integrating the most advanced technology to make sure that patient intake, coding, billing, reporting, and claims management are accurate will also help accelerate your facility’s revenue cycle management services. Harnessing technology’s wide array of abilities can reduce mundane and tedious administrative tasks for your staff while transforming information verification claims management and patient intake procedures.
Automate preregistration and registration
Automating stages of the revenue cycle management, such as the preregistration and registration phases, also drastically cuts down on the amount of time used to kickstart the process. By embracing automation throughout the different components of RCM, your facility can shift its focus from the details of billing and instead prioritize patient satisfaction practices, such as reducing wait times and exploring the best patient education methods to improve their health literacy.
Streamline patient communication
Additionally, using software to enhance communication with patients, offer convenient payment methods, and educate patients about the institution’s financial policies helps support fast and accurate billing practices that will stick out to patients.
Analyze RCM KPIs
Healthcare KPIs are another avenue to exploring the depths of the revenue cycle. Some specific KPIs to track include claims denial rates and payment collections, which can shine a light on areas for improvement.
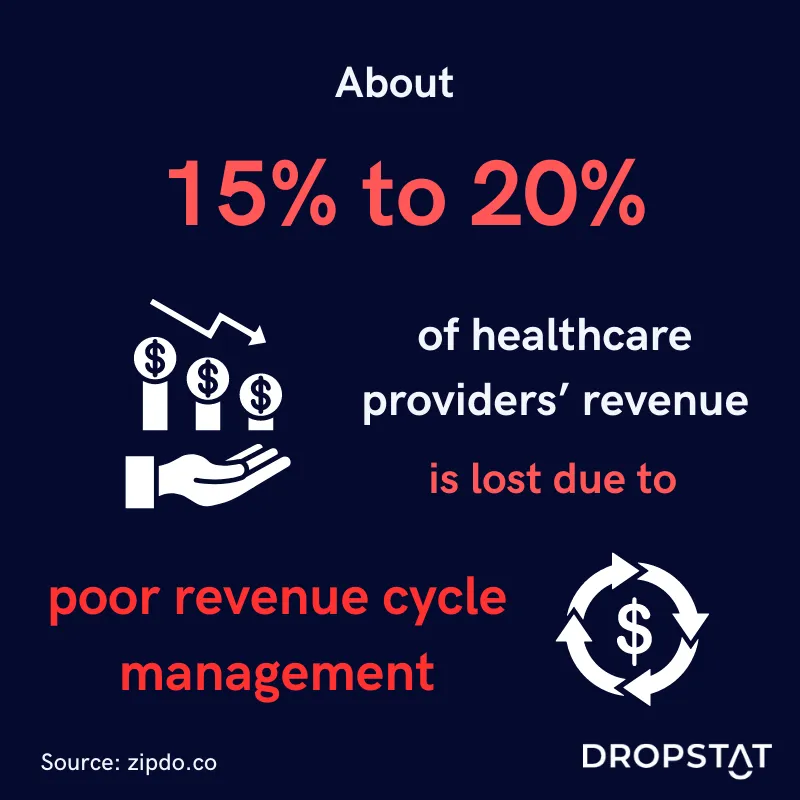
Challenges in health care revenue cycle management
Considering that revenue cycle management is impacted by a wide range of both people and procedures, acknowledging how they may pose challenges to this process is at the heart of optimizing its outcomes. Here are some examples of common challenges:
- The incredibly precise healthcare coding guidelines demand unique attention and vigilance. A lack of a high level of precision can lead to improper coding and increased denials.
- High turnover rates and poor employee satisfaction can be a barrier to training staff on new software and automation techniques and ultimately plays into the process of change management as well. Accepting new processes demands flexibility and trust from your staff.
- Compliance with the constant evolution of the healthcare ecosystem and patient responsibilities adds a layer of complication to processing.
However, navigating these barriers with the support of technology can lay the foundation for better revenue cycle outcomes.
How Dropstat simplifies healthcare revenue cycle management
With Dropstat, healthcare facilities can easily track specific KPIs such as overtime and bonus usage as well as shift-fill rate, which empowers schedulers and administrators to evaluate their staffing processes and how they impact revenue.
Ultimately, upgrading your staffing practices with Dropstat will lead to endless possibilities to devote more time to improving your revenue cycle, meeting employee needs, and increasing both employee and patient satisfaction. Schedule a demo with Dropstat now to start optimizing your staffing practices and generate more revenue.







