Telehealth nursing: What is it?
Telehealth nursing refers to the delivery of nursing care remotely using telecommunication technologies. Within the nursing profession, it is under the broader umbrella of telehealth, using technology in nursing to provide healthcare services from a distance.
Telehealth nurses leverage digital platforms to communicate with patients. These specially trained nurses assess patients’ health conditions, provide guidance, and offer support. Through videoconferencing, mobile apps, and other telecommunication tools, telehealth nurses bridge the gap between patients and healthcare providers, ensuring convenient and efficient care delivery.
Telehealth vs. telemedicine – the key differences
When comparing telemedicine vs. telehealth, the easiest way to define the difference is by viewing telemedicine as a subset of telehealth. It specifically refers to the remote delivery of clinical health services. Telehealthcare encompasses a broader scope, incorporating non-clinical healthcare activities facilitated by technology.
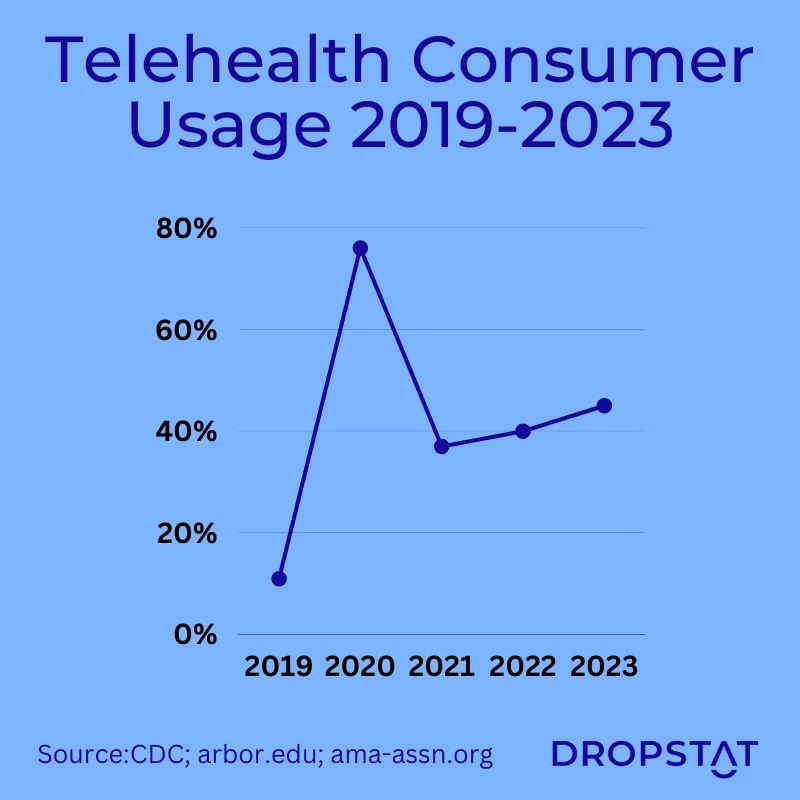
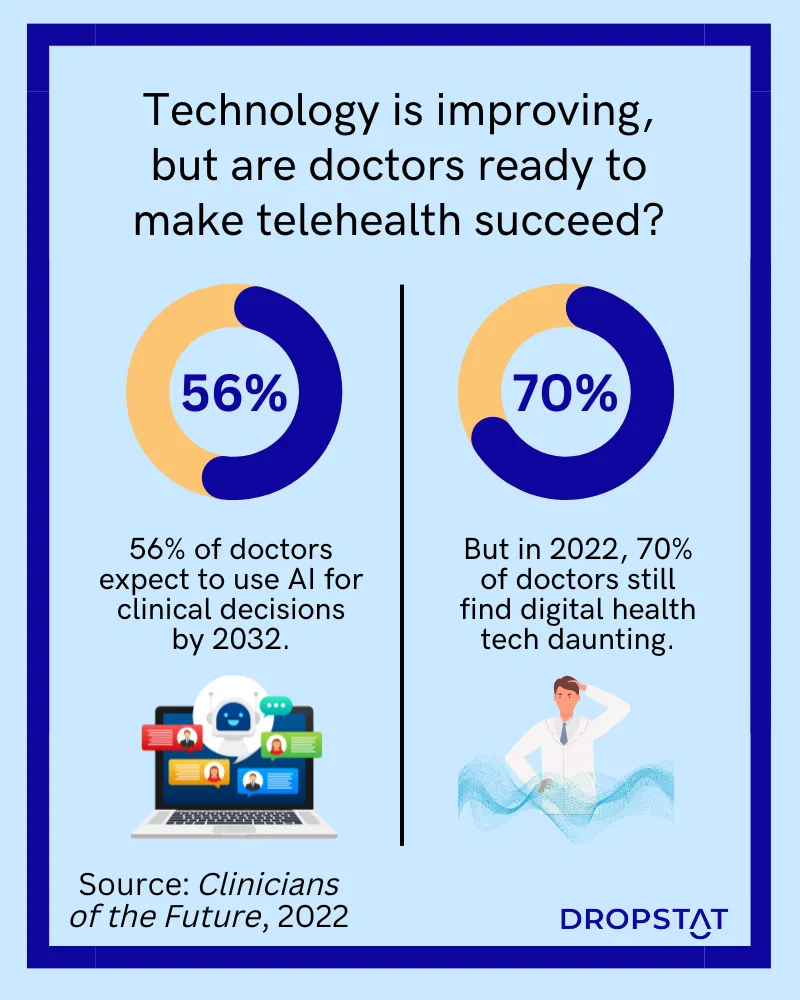
The popularity of telehealth rose greatly during the COVID-19 pandemic. After the intensity of COVID-19 passed, healthcare providers and consumers saw the benefits of telehealth for what they mean to healthcare facilities and the efficiency that can be harnessed. As technology continues to develop, we see that the partnership between healthcare and technology is here to stay.
What is telehealth?
“Telehealth” includes a broad spectrum of remote healthcare services, including telemedicine, tele education, and patient portal. Telehealth that takes place live, where the patient interacts with a provider via phone or video, is known as “synchronous telehealth.”
What is telemedicine?
“Telemedicine” definition is the provision of remote clinical services via two-way communication. Telemedicine encompasses remote diagnosis and treatment by physicians. The branches of telemedicine include;
- Interactive patient care – the use of technology to engage and involve patients in their own healthcare through interactive communication and educational tools.
- Remote patient monitoring – use of devices and technology to collect and transmit patient health data from a distance, enabling healthcare providers to monitor and manage patients remotely.
- Store and forward – a method of transmitting patient information, such as medical images or records, from one healthcare provider to another for consultation or analysis at a later time.
What is telehealth nursing?
“Telehealth nursing” refers specifically to nurses delivering care remotely. Telehealth nursing is part of telemedicine. Telehealth nursing is also referred to as telenursing and nursing telepractice.
What is the role of a telehealth nurse?
Telehealth RNs use telemedicine and technology to deliver nursing care to patients in remote locations. A telehealth nurse is the primary point of contact in telehealth nursing, assessing patients, providing guidance, and offering support via telecommunication technologies, such as providing telephone triage.
A telehealth nurse’s responsibilities include
- educating patients
- symptom management
- medication management, and
- remote patient monitoring, for example, by using electronic health records.
Through the capacity of telenursing, healthcare facility CEOs can achieve optimum facility efficiency, retain qualified registered nurses with less physical infrastructure, provide high-quality care, and extend the potential for improved patient outcomes. Telehealth nurses can care for more patients at once, increasing patient access without increasing the cost of medical care.
8 benefits of telehealth nursing for healthcare providers
Telehealth nursing enhances facility efficiency and improves quality of care. Here are 8 benefits for healthcare facilities:
1. Reduces staff workload and exposure
The telehealth setting alleviates the strain caused by nursing shortages and enables nurses to deliver medical care to a larger patient population with less physical strain. Telehealth nurses can provide care without being exposed to illnesses.
2. Reduces hospitalization and patient congestion
Telehealth nursing allows continuous monitoring, proactive interventions, and remote management of chronic diseases, for example, which reduces hospitalization of chronically ill patients, which reduces patient congestion in the facility.
3. Enables provision of healthcare
Healthcare providers can provide medical care and consultations by telehealth nurses from remote locations, enhancing the provision of quality care.
4. Increases financial savings for healthcare facility
Telehealth nursing reduces costs associated with in-person caregiving, transportation of caregivers, and emergency department personnel, resulting in substantial financial savings for healthcare facilities. There is also increasing governmental support through reimbursement via telehealth CPT codes; some healthcare facilities hire telehealth and RPM reimbursement specialists to assist in the reimbursement process.
5. Improves bed allocation
By providing timely remote medical care and proactive interventions, telehealth nursing helps reduce unnecessary hospital admissions, which optimizes bed allocation and ensures efficient resource allocation.
6. Enhances the reputation of the healthcare facility
Through telehealth nursing, healthcare facilities offer personalized medical care in the patient’s familiar surroundings, which provides a better patient experience, and results in a better reputation for the healthcare facility.
7. Increases employment opportunities
Telehealth nursing opens new avenues for healthcare facilities to hire top talent for remote care providers. This expands healthcare employment opportunities and addresses workforce demands. Nurses can provide care during traditional clinic hours and outside regular working hours to accommodate patient needs and provide telehealth services across time zones, subject to out-of-state licensing requirements.
8. Expands healthcare liaison and efficiency
Telehealth nursing increases liaison and communication between remote members of the healthcare team for better delivery of medical care. This improves the efficiency of the whole healthcare team.
By welcoming telehealth in nursing, healthcare facility CEOs can achieve facility efficiency, enhance quality medical care, and ultimately transform and simplify the healthcare experience for healthcare providers.
How to successfully hire a telehealth nurse
Before beginning a new telehealth program, or when evaluating the success of an ongoing telehealth program, look at recommendations on the American Telemedicine Association (ATA) website and the American Nurses Association (ANA) website as it applies to your healthcare facility.
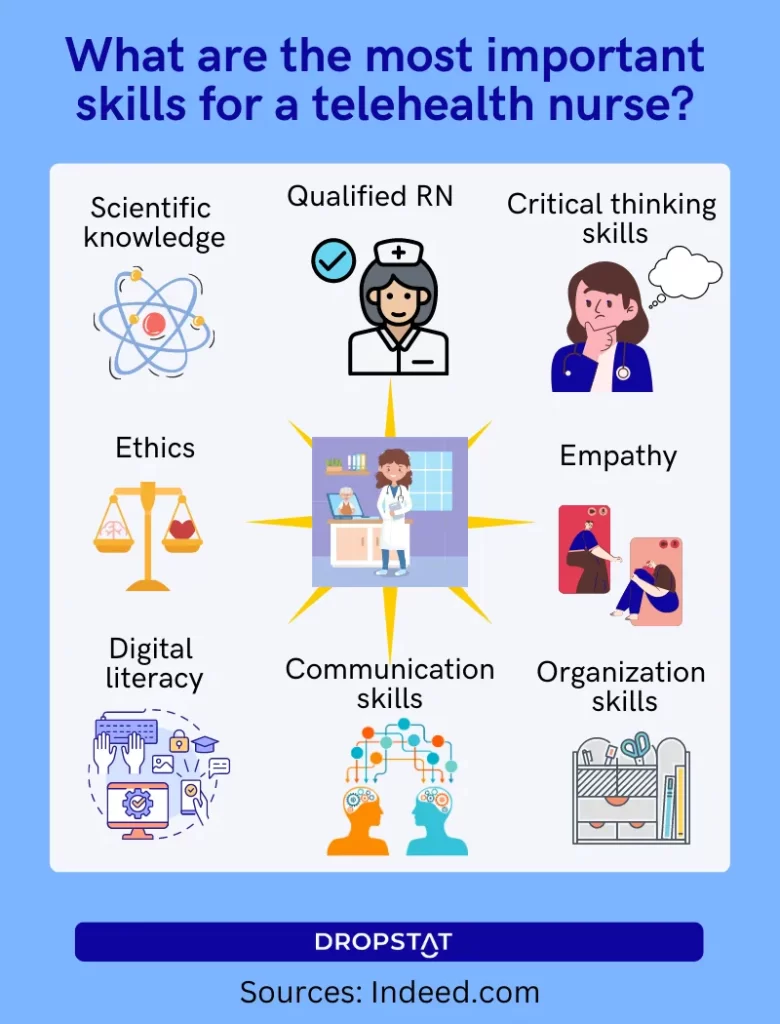
A telehealth nurse candidate must possess a Bachelor of Nursing degree that qualifies them as a registered nurse (RN). The Ambulatory Care Nursing Certification (RN-BC) is another type of certification that is popular. The nursing licensure certification must be for the relevant state/s telehealth nurses will work in. In addition to skills that a registered nurse requires, telehealth RNs require
- excellent communication skills
- perspective-taking skills
- an ability to ‘translate’ medical jargon into simple terms via telecommunications technology or via a video call
- competence in using technological platforms
- be comfortable communicating through technology
A telehealth nurse must also demonstrate ethics, patience, and empathy. A certified telehealth nurse must show extended experience – commonly 5 years.
Telehealth nurse salary
Determine the salary you will offer. As of 2023, a telehealth nurse’s salary averages $66,559 according to ZipRecruiter (national average); however, Salary.com points out that a telehealth nurse’s salary usually depends on a telehealth nurse’s years of experience and skills and can be more than $111,696 per annum.
Telehealth nurses work can work up to 12-hour shifts like many other nurses, 30-40 hours a week for full-time and 16-29 hours a week for part-time positions. Some full-time telehealth RNs are eligible for telehealth benefits, including health insurance, holiday pay, continuing education, and paid time off (PTO).
7 examples of modalities that telehealth nursing uses
Telehealth nursing encompasses various options that enable remote healthcare delivery. Here are examples of the types of telehealth nursing available.
1. Live video conferencing: Nurses engage with patients in actual time through secure video platforms, providing assessments, consultations, and professional health-related education. Nurses can use synchronous telehealth to offer basic consultations for acute or chronic care.
2. Phone consultations: Nurses connect with patients over the phone, offering guidance, triage services, and answering health-related questions.
3. Email communication: Nurses interact with patients via email, addressing non-urgent inquiries, sharing resources, and facilitating follow-up care.
4. Remote patient monitoring: Nurses utilize technology to monitor patients’ vital signs, and symptoms, and collect health data remotely, allowing for proactive interventions and early detection of health issues.
5. Mobile health (mHealth) applications: Nurses leverage smartphone apps and wearable devices to communicate with patients, deliver educational materials, track progress, and provide ongoing support.
6. Store-and-forward: Nurses receive patient information, such as medical records, diagnostic images, or lab results, electronically and review them later, providing assessments, recommendations, or consultations.
7. Virtual clinics: Nurses run virtual clinics or online platforms where patients can seek medical advice, receive prescriptions, and schedule appointments with healthcare professionals.
By incorporating these different types of telehealth nursing into healthcare facilities, CEOs can expand their service offerings, improve patient access and engagement, and enhance overall efficiency while maintaining the highest standards of quality medical care.
Areas of telehealth nursing practice
Telehealth nursing is poised to have a significant impact on healthcare, as the growth of telehealth, in general, has paved the way for improvement in diverse telenursing practice areas. These emerging fields include:
1. Telepediatrics: Remote healthcare services catering specifically to pediatric patients, including consultations and monitoring.
2. Telecardiology: Remote diagnosis, monitoring, and management of cardiac conditions, enabling timely interventions.
3. Telehomecare: Remote monitoring, education, and support for patients who manage chronic conditions from their homes.
4. Telestroke: Rapid evaluation and treatment of stroke patients through remote consultation and imaging analysis.
5. Teletrauma: Immediate virtual trauma assessment and support for time-sensitive interventions.
6. Teletriage: Remote assessment and prioritization of patient needs to determine appropriate levels of triage care. Studies show that remote triage reduces the burden on primary care and emergency departments.
7. Forensic telenursing: Utilizing telehealth technologies to support forensic nursing practice, including evidence collection and documentation.
8. Telemental health: Remote mental health support, counseling, and therapy sessions are provided through secure digital platforms.
9. Tele ICU: Remote monitoring and critical care support for intensive care unit patients.
10. Telerehabilitation: Virtual therapy sessions and remote monitoring for patients undergoing rehabilitation treatments.
These areas of telenursing practice showcase the expanding scope and potential of telehealth nursing to deliver specialized care remotely.
How Dropstat complements healthcare facilities that offer telehealth nursing
Dropstat, an AI-powered scheduling software, can help optimize scheduling for telehealth nurses who work in a healthcare facility or work remotely in different locations. As healthcare advances with telehealth in nursing, Dropstat allows healthcare schedulers to efficiently allocate nursing resources across various healthcare locations, ensuring appropriate staff coverage for a healthcare facility’s telehealth services.
Dropstat’s app includes a master schedule and an individual schedule for every shift. The scheduler and the nurse managers can immediately see whether all shifts are fully staffed and that in-house and remotely-located telehealth nurses are working. This enables healthcare facilities to maintain efficiency, provide continuous quality care, and satisfy regulations.
Dropstat facilitates flexible scheduling that aligns with the needs of nurses and clinicians, optimizing availability and accessibility. By streamlining the scheduling process, CEOs can maximize efficiency, reduce administrative burdens, and enhance quality care delivery through telehealth nursing, ultimately adapting the healthcare facility to the special demands of an evolving industry.
Schedule a demo to learn more about Dropstat’s cutting-edge scheduling tool.







