What is nursing handoff?
Nursing handoff is the process that occurs when one team of nurses hands over responsibility for patient care to the team of nurses on the next shift. It is essential to make sure that the transfer of patient care information is efficient and accurate.
Handoff communication can take place between teams or individuals of physicians and nurses. The nursing handoff report discusses patient care that took place recently and care that is expected. Interactive communication between nursing shifts at handoff time allows information about patients to be shared, verified, and contributed to.
The importance of nursing handoff report: A transfer of responsibility
Nursing care takes place around the clock. Each nursing shift is responsible for providing care until shift handoff. An essential part of successful nursing handoff is the accurate communication of patient information to the next shift. This is done via a handoff report given from the outgoing team or nurse to the incoming team or nurse. It is critical that the handoff report is an accurate and comprehensive report of the patient’s progress during the shift that ended. This is an essential link in the continuity of care for each patient.
ACOG sees hospital care as being in an “era of collaborative care.” Various medical teams handle different aspects of patient care. Effective shift-to-shift handoff helps avoid medical errors and improves patient safety while cultivating a medically excellent environment. Good communication between nurses and other medical personnel at handoff is one of the most important components of this collaborative effort.
Responsible nursing handoff is crucial to patient safety and outcomes
Patient safety
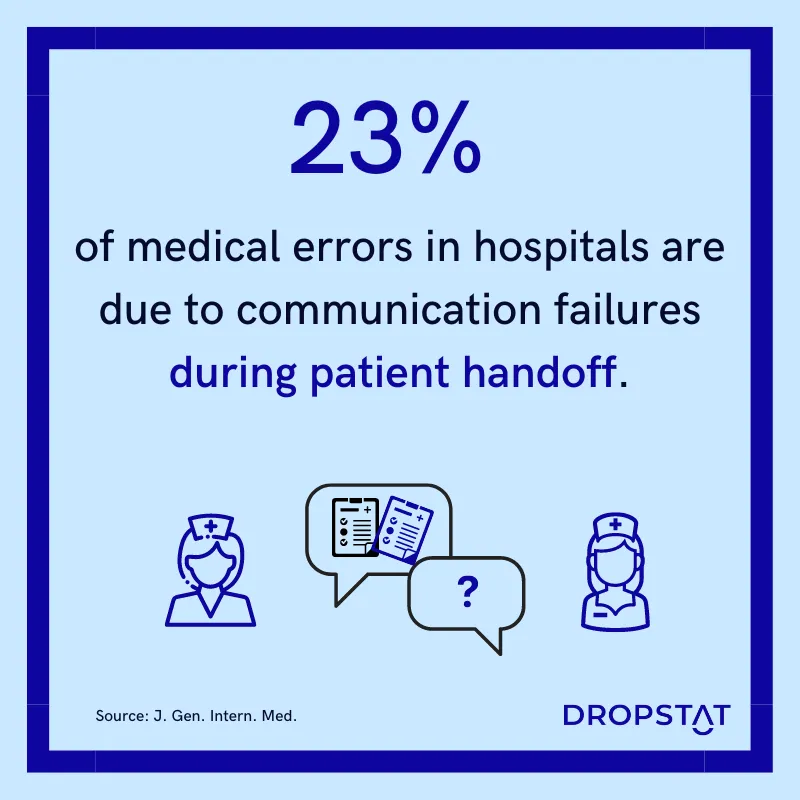
A leading cause of medical errors is inaccurate communication of patient care. Handoff communication failures are the cause of 80% of medical errors, according to a Joint Commission report. A 2005 study published in the Annals of Internal Medicine found that communication errors were a contributing factor in 37% of medication errors in the intensive care unit and that the majority of these errors (65%) were related to handoffs between healthcare providers.
Patient outcomes
Good patient outcomes depend on nurses communicating medical details accurately at handoff. A study published in the Journal of General Internal Medicine found that patients who experienced communication failures during their hospital stay had a 30% higher risk of being readmitted within 30 days of discharge. On the other hand, resident physicians saw a 23% reduction in medical errors and a 30% reduction in preventable adverse effects when they used a structured handoff report.
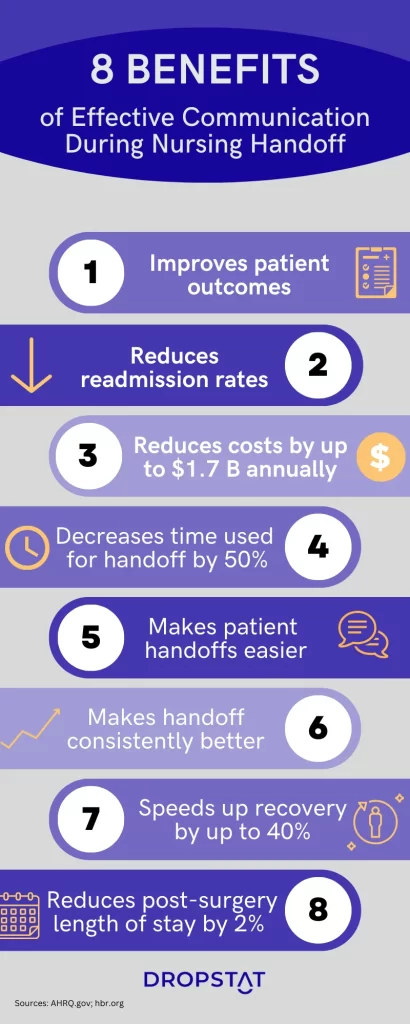
Benefits of effective patient handoff:
- Fewer delays in patient care
- Reduced care costs
- Reduction in care omissions and medical errors
- Reduced length of hospital stay
- Reduced readmission rates
- Clarity of patient care requirements
- Improved patient safety
- Improved patient care and outcomes
Effective handoff communication skills
Hospital managers want a culture of open communication, collaboration, and teamwork between nurses for quality patient care and patient satisfaction. Furthermore, clinical routine relies upon clear, reliable communication between staff members, as teams hand off patients at the end of the shift.
Skills that nurses need for effective handoff communication:
- Being present and focused
- Ability to give a concise, organized, end-of-shift report
- Awareness of the most important pieces of information to give
- Use of standardized medical terminology
Oncoming nurses contribute to the handoff procedure by
- Being punctual
- Listening to the report carefully, with focus
- Asking questions if there is time
Overcoming barriers in handoff communication
In healthcare communication, barriers at nursing handoff commonly include:
- Nurses not informing their manager in advance that they will be absent from their shift.
- Shift members not being punctual for shift start.
- Conflicts and defensiveness between staff members.
- Negative organizational culture due to organizational disarray.
- Personnel hierarchies cause intimidation of junior staff members, who are afraid to point out possible errors of senior staff.
- Different communication styles due to no streamlined system of messaging staff.
- Fatigue due to nurse overtime obligations.
Many of these barriers to communication can be overcome by the systematic organization, such as effective shift scheduling and effective communication in nursing.
Healthcare personnel can also overcome medical communication barriers with the following:
- Standardizing nursing handoff reports
- Training staff in patient handoffs
- Supplying necessary tools and resources

3 types of nursing handoff reports
The best setup for doing nursing handoff reports is at a routine time, with an agreed customary procedure. Using a standardized approach for the nursing handoff report makes the transfer of the information far more accurate, complete, and reliable.
Three popular nursing handoff reports are:
- SBAR nurse handoff for bedside shift reports. ASQ.org provides an SBAR nursing handoff example.
- TeamSTEPPS program for nursing shift reports
- I-PASS for verbal handoff reports
Verbal nursing shift report
A verbal nursing shift report is a face-to-face communication that takes place between the outgoing nurse(s) providing a report to the incoming nurse(s) about the patients in their care.
During the verbal shift report, the outgoing nurse(s) will typically provide information about each patient’s condition, any changes in their status since the last shift, medications given, procedures performed, and any concerns or issues that need to be addressed. It is a perfect opportunity for patients to ask questions about their care and offers insights to help the healing process.
Written nurse handoff report
A written nurse handoff report is a document that is used to communicate patient information and can be referred to throughout the shift. The report typically includes information such as the patient’s diagnosis, medical history, current medications and treatments, vital signs, and any relevant test results or procedures.
The written nurse handoff report may also include information about the patient’s care plan and goals and any special instructions or considerations that the incoming nurse(s) should be aware of.
Written communication, in the form of organized charts – either manual or electronic – presents an opportunity for a more organized presentation of important details. If it is printable, the incoming team will have a useful hard copy for reference, further reducing space for medical errors. Electronic handoff information has a big plus, however – legibility. Illegible handwriting is a proven cause of medical errors.
Bedside shift report
A bedside shift report takes place at the patient’s bedside. This method is designed to improve patient safety and increase patient engagement in their own care by involving them in the handoff process.
During a bedside shift report, the leaving and starting nurses discuss the patient’s care plan with the patient present. This allows the patient to ask questions, provide input, and become more involved in their own care.
Bedside shift reports ensure that important information is not missed or misunderstood, as the patient and both nurses can clarify any details or concerns. Studies show that when patients are involved in their health plans, patient outcome is improved.
The bedside report does not cancel out the need for other staff meetings regarding patient care, for example, those taking place in a conference room or in a quiet and private setting.
Key components of handoff communication
There is no universally-accepted nursing handoff protocol. However, certain key elements should be included:
- personal demographic information
- brief medical history
- findings of the physical examination
- list of the patient’s medical problems that are currently being treated
- tests are already done, awaiting results
- anticipated care program
- anything of key importance to the patient
- any other important information
Patient information that is static and documented elsewhere is not included in the nursing handoff report:
- Non-essential patient comorbidities
- An entire list of patient medications
- Patient’s lab results
Dropstat’s essential contribution to effective nursing handoff
Dropstat’s encrypted internal chat system between the nurse manager and nurses means that if a staff member cannot make it for their shift, they can instantly communicate with their manager. Nurse managers can see in real-time which nurses have been scheduled for each shift and keep tabs on nurses who consistently arrive late for their shift – a factor that could be detrimental to nursing handoff.
Dropstat’s staff communication system also boosts effective, positive communication between staff, especially amongst nurses at shift changes. Staff can infuse a day with positivity using the Dropstat gratitude feed. Positivity has been proven to improve communication in every healthcare setting. With a friendly organizational culture featuring support and acceptance, staff will be friendlier to each other and ultimately communicate more effectively at nursing handoff.
Schedule a demo with Dropstat to see how you can schedule shifts for your staff that promote great communication and excellent nursing handoff reports.







